指南解读|你知道结直肠癌“四大争论”吗?新版CSCO结直肠癌诊治新指南为您解惑!
2018-05-14 蔡三军 李心翔 医师报
CSCO结直肠癌诊疗指南2018.V1基于循证医学证据和精准医学基本原则,充分考虑我国结直肠专科医师需求和肠癌诊疗现状,并且结合中国国情和不同地区经济发展水平差异,对指南进行了相应更新,将2017版中的“基本策略”和“可选策略”统一修改为“Ⅰ级”、“ Ⅱ 级”和“Ⅲ级”专家推荐,并标注了医学证据水平。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新指南#
74
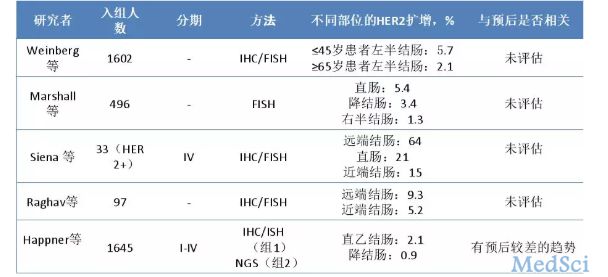
结直肠癌靶向药物治疗.
98
#结直肠#
71
#指南解读#
67
很棒.谢谢
0
了解了谢谢
93
谢谢分享学习
106