我国学者在糖尿病缺血性血管疾病发生机制方面的研究取得重要进展
2017-02-14 朱元贵、郭峻莉、江虎军 医学科学部
在国家自然科学基金项目(项目编号:91639111,81573435)等资助下,温州医科大学中美糖尿病并发症研究所谭毅研究组在糖尿病缺血性血管疾病发生的调控机制研究中取得重要进展。相关研究成果以“Elevating CXCR7 Improves Angiogenic Function of EPCs via Akt/GSK-3β/Fyn-Mediated Nrf2 Activation in Di
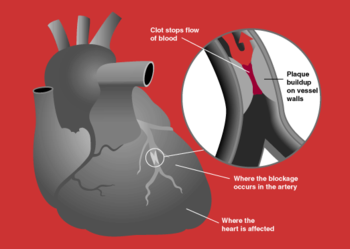
血管并发症是糖尿病患者致残和致死的主要原因。糖尿病血管并发症主要是由糖尿病氧化损伤所致血管重塑和血管生成功能失调、对缺血/缺氧刺激的反应性降低、血管修复功能受损或异常引起的。内皮祖细胞(endothelial progenitor cells,EPCs)在血管再生过程中起关键作用,但糖尿病能够导致外周EPCs数量减少、血管形成功能受损,其机制至今未明。谭毅教授的研究团队前期研究发现,基质细胞衍生因子(SDF-1)受体CXCR7在EPCs细胞膜上表达,并且参与EPCs的存活、增殖、粘附、跨内皮迁移和血管形成等重要病理生理过程。该团队与合作者进一步研究发现,糖尿病小鼠(db/db)体内的EPCs或体外高糖/高脂处理后的EPCs,CXCR7表达均显着降低,并伴随氧化损伤、凋亡和血管形成功能受损;慢病毒介导CXCR7过表达可显着抑制上述病理变化,并有效促进糖尿病缺血性血管再生和血流恢复。进一步机制研究表明,CXCR7的保护效应主要通过Akt/GSK-3β/Fyn信号途径介导抗氧化转录调节因子Nrf2的核转位和转录激活,从而增强EPCs的抗氧化和血管生成能力。该研究表明,糖尿病诱导的CXCR7下调是糖尿病导致EPCs功能障碍的主要原因,趋化因子受体CXCR7和转录调节因子Nrf2可能是治疗糖尿病缺血性血管疾病的重要靶点。
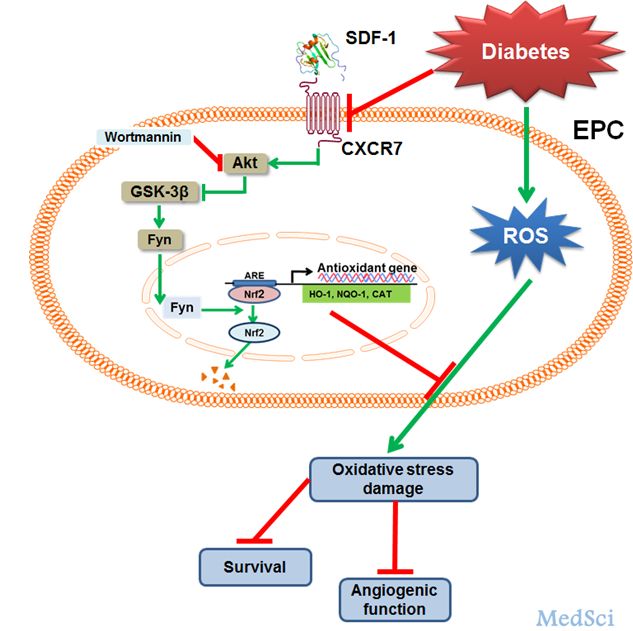
参考文献:Xiaozhen Dai,Xiaoqing Yan,Jun Zeng,et al.Elevating CXCR7 Improves Angiogenic Function of EPCs via Akt/GSK-3β/Fyn-Mediated Nrf2 Activation in Diabetic Limb Ischemia.Circulation Research.January 30.2017
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#我国学者#
87
#重要进展#
68
#缺血性#
73
创新性强
90
#血管疾病#
60
#发生机制#
57