科学家首次获得具有功能的精子细胞
2016-03-01 周琪等 《细胞—干细胞》
近日,以中科院动物研究所周琪院士为首,南京医科大学沙家豪教授和中科院动物研究所赵小阳教授(现南方医科大学教授)参加的合作团队,首次实现干细胞体外减数分裂获得具有功能的精子细胞,相关成果发表在2月25日的《细胞—干细胞》上。 该团队致力于利用干细胞技术研究配子发生障碍等生殖医学问题,利用基因编辑技术纠正遗传突变,可以使无精子症小鼠恢复生育能力。但这个过程需要将原始生殖细胞移植到睾丸中继续分化,而其
近日,以中科院动物研究所周琪院士为首,南京医科大学沙家豪教授和中科院动物研究所赵小阳教授(现南方医科大学教授)参加的合作团队,首次实现干细胞体外减数分裂获得具有功能的精子细胞,相关成果发表在2月25日的《细胞—干细胞》上。
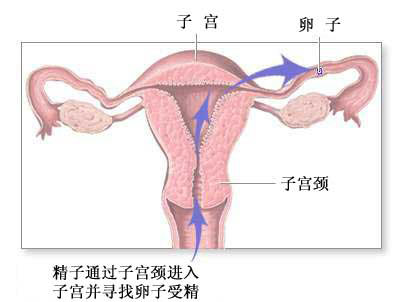
该团队致力于利用干细胞技术研究配子发生障碍等生殖医学问题,利用基因编辑技术纠正遗传突变,可以使无精子症小鼠恢复生育能力。但这个过程需要将原始生殖细胞移植到睾丸中继续分化,而其中可能会残留少量的多能性干细胞混合在原始生殖细胞中,经过移植后可能有致瘤的风险,因此在人类中的研究以及未来的临床应用都存在问题。
那是否有可能在体外实现减数分裂过程呢?这一问题是生殖发育研究领域科学家的一个梦想,但由于减数分裂过程本身极为复杂,受到机体的多种信号调控,多年来没有大的突破。
据了解,该团队结合干细胞技术、基因编辑技术等,精心设计了一个研究方案,经过两年多的尝试,分步解决了其中的主要问题,建立了一个全新的生殖细胞体外分化系统,使小鼠胚胎干细胞体外分化获得精子。
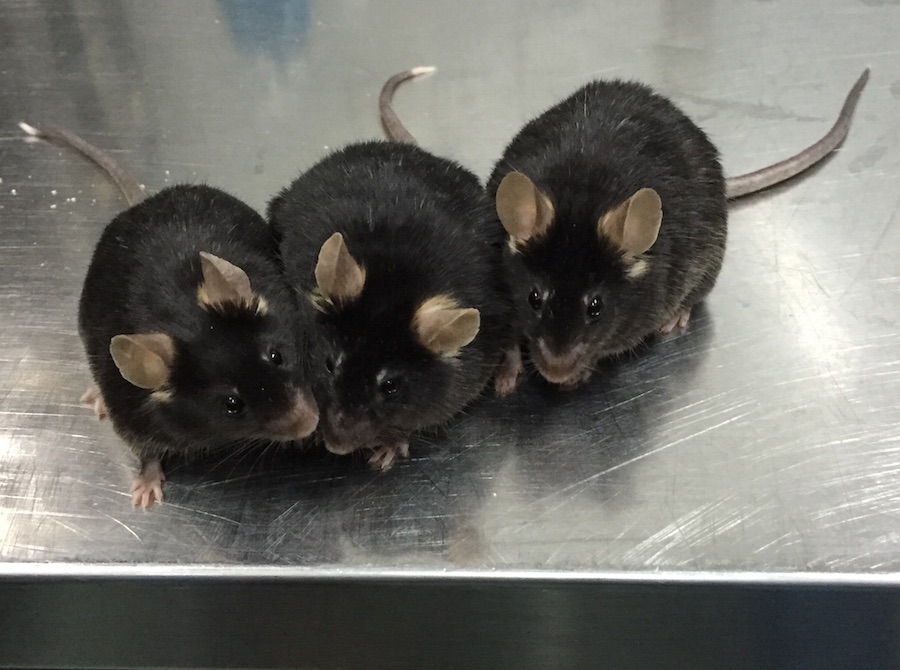
与之前的研究不同的是,该研究首次在体外重现了生殖细胞的减数分裂过程,与体内减数分裂过程基本类似,其所获得的精子具有受精能力,能够获得健康的后代,该技术有望帮助无精子症男性获得后代。到目前为止,该技术已经在项目内多个研究组得到重复,产生了数十只小鼠后代,这些小鼠发育良好,并且可以正常繁殖下一代。
赵小阳教授提出,该研究实现了生殖发育领域的一个重大突破,为人类生殖细胞体外分化奠定了理论基础,为解决人类不孕不育问题提供了新的思路。该技术避免了原始生殖细胞体内移植的步骤,回避了移植过程可能引起的致瘤风险,具有良好的应用前景。由于该研究使得体外研究哺乳动物减数分裂成为可能,从而为研究者提供了一个新的研究平台,将加速减数分裂的机制研究和针对不孕不育症的规模化药物筛选。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












真的不错
92
牛逼
101
很不错
122
有很好
126
继续
72
突破
103