Stroke : 华西医院新发现:无症状的烟雾病,有何临床特点?
2021-09-29 Freeman MedSci原创
MMD中三种类型的无症状半球是确定的,具有独特的血管学和血流动力学特征
Moyamoya病(MMD)是一种慢性脑血管疾病,在1957年首次被描述为双侧Willis环的主要分支和基底神经节区域的烟状血管网的进行性狭窄或闭塞。颅内出血和脑缺血是主要的发病形式;其他常见形式包括继发性癫痫和认知障碍。根据定义,MMD可以影响患者的左、右半球。然而,事实上,并非所有的MMD患者都出现双侧症状,这就强调了MMD中的症状半球和无症状半球的概念。

目前MMD的治疗主要是通过脑血管重建手术(颅内外搭桥手术、间接血管重建或联合血管重建)治疗有症状的半球,以改善脑灌注。然而,MMD中无症状的半球过去被认为是无症状的,没有引起足够的重视。
但据报道,无症状半球在病程失代偿期的某个时候可以发展为有症状半球,并带来不可逆的脑损伤。在日本进行的第一次全国性多中心调查,重点是无症状的MMD患者,报告说每年有3.2%的中风风险。
此外,随着磁共振检查的广泛使用,无症状MMD的发病率可能比以前认为的要高。因此,需要对无症状的半球进行更好的描述,以指导管理策略。
藉此,华西医院的Haogeng Sun等人,回顾了MMD患者中无症状和有症状半球的临床和影像学特征,重点是关于血管形态和脑灌注的影像学特征。然后,定义了3种类型的无症状半球,并研究了它们的差异以及它们与有症状半球的关联。
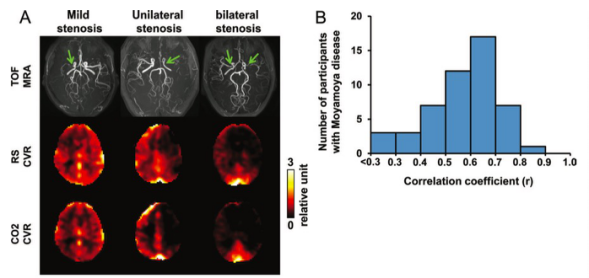
他们回顾单中心MMD患者连续病例中无症状和有症状的半球的临床和影像学特征,重点是关于血管形态和脑灌注的影像学特征。MMD半球被分为5种类型:出血性半球、缺血性半球、单侧出血性MMD的无症状半球、单侧缺血性MMD的无症状半球以及MMD的双侧无症状半球。血管造影特征由Suzuki的血管造影阶段来评估,而血流动力学特征由梗死前时期阶段来评估。
他们纳入了194名MMD患者,累及共388个半脑。单侧出血性MMD的无症状半球与出血性半球基本相似,与MMD的双侧无症状半球和单侧缺血性MMD的无症状半球相比,两者的Suzuki血管造影阶段更晚,血流动力学衰竭程度更低。
单侧缺血性MMD的无症状半球与缺血性半球相似,与MMD的双侧无症状半球和单侧出血性MMD的无症状半球相比,
两者的Suzuki血管造影阶段较低,血流动力学失败程度较高。MMD的双侧无症状半球与其他半球不同,其Suzuki的血管造影阶段较晚,血流动力学衰竭程度较低。
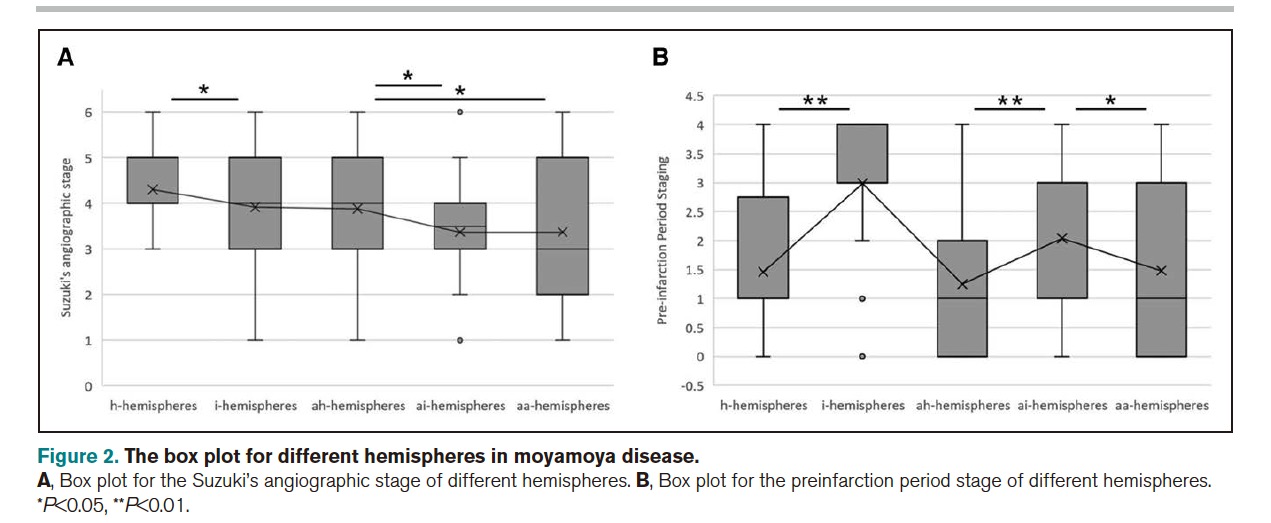
这个研究的重要意义在于发现了:MMD中三种类型的无症状半球是确定的,具有独特的血管学和血流动力学特征。这两个特征的不同组合可以反映这些不同无症状半球的病理演变趋势。
原文出处:
Sun H, Li W, Xia C, et al. Angiographic and Hemodynamic Features in Asymptomatic Hemispheres of Patients With Moyamoya Disease. Stroke. Published online September 22, 2021. doi:10.1161/STROKEAHA.121.035296
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#西医院#
92
#新发现#
142
#临床特点#
117
#华西#
139
#无症状#
125