盘点:系统性红斑狼疮近期重要研究进展一览
2017-07-10 MedSci MedSci原创
系统性红斑狼疮是一种自身免疫疾病,以产生多种自身抗体、以产生多种自身抗体、免疫系统异常激活为特点,累及全身多个组织器官。如果病情得不到控制,将会导致器官衰竭,甚至早亡,对患者身心健康造成巨大影响。这里梅斯小编整理了近期关于系统性红斑狼疮的重要研究进展于大家一同分享。【1】Heart:系统性红斑狼疮患者心力衰竭的发生率及风险如何?虽然系列病例表明相比于普通人群,系统性红斑狼疮患者具有较高的心血管
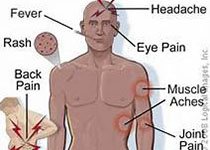
系统性红斑狼疮是一种自身免疫疾病,以产生多种自身抗体、以产生多种自身抗体、免疫系统异常激活为特点,累及全身多个组织器官。如果病情得不到控制,将会导致器官衰竭,甚至早亡,对患者身心健康造成巨大影响。这里梅斯小编整理了近期关于系统性红斑狼疮的重要研究进展于大家一同分享。
【1】Heart:系统性红斑狼疮患者心力衰竭的发生率及风险如何?
虽然系列病例表明相比于普通人群,系统性红斑狼疮患者具有较高的心血管风险因素。然而,系统性红斑狼疮和心力衰竭之间的相关性尚不明确。近日,在心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员旨在探讨系统性红斑狼疮患者的心衰的发病率和风险。
在有45284540名参与者的数据库中,研究人员确定了95400(0.21%)名已有系统性红斑狼疮患者和98900(0.22%)名在2015年5月至2016年4月期间新近诊断的心衰患者。
研究人员发现心衰发生率在系统性红斑狼疮患者中明显高于对照组,以及其他心血管危险因素也一样的高。在回归分析中,系统性红斑狼疮是心力衰竭的独立预测因子。在年轻男性系统性红斑狼疮患者中心衰相对危险度最高,并且绝对风险总体趋势也有所增加,但在男性和女性中,随着年龄增加相对危险度逐渐下降。累及肾脏的系统性红斑狼疮与心衰较早发生和较高发病率有关。(文章详见——Heart:系统性红斑狼疮患者心力衰竭的发生率及风险如何?)
【2】Arthritis Rheum:羟氯喹对皮肤型红斑狼疮患者安全有效
羟氯喹(HCQ)是一种抗疟药,也是一种独特的抗风湿病药物。2017年4月,发表在《Arthritis Rheumatol》的一项研究显示,羟氯喹对皮肤型红斑狼疮安全有效。
研究者开展了一项双盲、随机、平行组临床试验,一共纳入103名活动期CLE患者。在16周双盲期内,按3:1比例将患者随机分配至接受HCQ或安慰剂,在随后的36周单盲期内,所有患者被给予HCQ。
结果,在HCQ组和安慰剂组中,从基线起16周平均CLASI得分均显着改善:平均变化为-4.6和-3.2,并且没有组间差异(P=0.197)。调查者的整体评估显示HCQ组中“改善”和“显着改善”患者的百分比较大。其他次要终点也证实了HCQ的疗效。蜂窝织炎、药疹、肝功能障碍和Stevens-Johnson综合征是HCQ使用的严重不良事件。(文章详见——Arthritis Rheum:羟氯喹对皮肤型红斑狼疮患者安全有效)
【3】Rheumatology:系统性红斑狼疮怀孕女性的药物使用情况
系统性红斑狼疮(SLE)疾病本身并不影响女性患者的生育能力,但病情活动需要用药。2017年4月,发表在《Rheumatology (Oxford)》的一项研究显示,在近一半的SLE孕妇中,女性被处方DMARDs和CSs。
从瑞典医学出生注册库(2006~2012)中识别出妊娠结局为活产或死胎的女性。采用全国注册库识别出怀孕期有和没有SLE的女性,并且识别出孕前3个月至产后6个月的药物处方。研究者报道了SLE孕妇中DMARDs、系统性CSs和NSAIDs的流行率(单独报道阿司匹林)。研究者计算了怀孕期内处方给≥5%的SLE孕妇的其他药物的流行估算值,以及无SLE孕妇的相同药物。
结果,SLE女性中有483名孕妇,无SLE女性中有5723名孕妇。在SLE孕妇中,49.3%在怀孕期内使用1种或以上的DMARDs,CSs的使用率是48.0%,阿司匹林是40.8%,其他NSAIDs是6.0%,并且在不同怀孕期内是不同的。SLE孕妇中常用药物的使用率比无SLE孕妇高1.2至20倍。(文章详见——Rheumatology:系统性红斑狼疮怀孕女性的药物使用情况)
【4】Arthritis Rheumatol:贝利单抗皮下给药:系统性红斑狼疮患者的福音?
2017年5月,发表在《Arthritis Rheumatol》的一项为期52周的随机、双盲、安慰剂组对照研究表明,贝利单抗SC给药治疗SLE有效且安全。
按2:1随机分为每周用预充注射器贝利单抗SC给药200mg组或安慰剂组。839名随机患者中,836名(贝利单抗组556名和安慰剂组280名)接受治疗。共有159名患者在研究结束前退出。开始时,贝利单抗组平均SELENA-SLEDAI评分是10.5,安慰剂组是10.3。
与接受安慰剂的患者相比,贝利单抗组中更多患者有SRI4应答。在40~52周期间,与安慰剂组相比,贝利单抗组中严重耀斑的时间和风险皆有改善,更多患者能减少糖皮质激素剂量≥25%。治疗组之间的AE发病率相当;10.8%使用贝利单抗的患者和15.7%接受安慰剂的患者报告严重的AEs。0.9%使用贝利单抗的患者和1.4%接受安慰剂的患者发生≥2级的IgG低球蛋白血症恶化。(文章详见——Arthritis Rheumatol:贝利单抗皮下给药:系统性红斑狼疮患者的福音?)
【5】Arthritis Rheumatol:系统性红斑狼疮的生物标志物-一种新方法减轻免疫抑制剂的干扰
分子医学的发展提高了人们对系统性红斑狼疮(SLE)中靶向生物制剂的期望,但临床试验的结果令人失望,并难以解释。研究人员进行狼疮生物标志物研究以测试停用免疫抑制剂,作为使SLE试验可以解释的新方法。
在41例活动性非器官威胁性SLE急性发作患者(A组)中,给予了临时类固醇而免疫抑制剂被停药。评估丧失抑制疾病的时间(疾病发作时间)和安全性。当症状复发时,立即恢复标准治疗。通过多重测定、酶联免疫吸附测定和信使RNA阵列研究了基线时A组患者和另外62名捐赠样本的患者(B组)的标准治疗免疫学影响。
具有较低或较高基线疾病活动的患者疾病发作中位时间分别为71和45天;6个月时41例患者中有40例(98%)出现急性发作。所有发作在6周内得到治疗和解决。从发作或感染中没有发生严重的不良事件。I型干扰素(IFN),Th17和B淋巴细胞刺激因子通路一致。基线免疫抑制剂对Th17和B淋巴细胞刺激因子具有明显的影响,这取决于IFN特征。(文章详见——Arthritis Rheumatol:系统性红斑狼疮的生物标志物-一种新方法减轻免疫抑制剂的干扰)
【6】Ann Rheum Dis:他汀类使用者中系统性红斑狼疮的风险模式
这项研究旨在分析使用他汀类药物与患系统性红斑狼疮( SLE)风险之间的关联,重点是描述随时间变化的风险模式。
参与者为所有在1995-2009年期间至少服用一种他汀类药物并且年龄在40岁以上的患者,根据年龄,性别和首次处方日期与非使用者进行匹配。他汀类使用者的随访期被分为目前、近期和过去暴露期,随着时间的推移,患者在这三种暴露类别之间转换。目前的他汀类使用者也被分为使用≤1年或> 1年。
共纳入了1 039 694例患者,其中519 847例为他汀类使用者。在40岁以上的患者中目前的他汀类使用者患SLE的风险没有增加。持续治疗1年以上的他汀类使用者发生SLE的风险降低了38%。然而,当使用SLE更具体的定义时后一个发现没有被观察到。(文章详见——Ann Rheum Dis:他汀类使用者中系统性红斑狼疮的风险模式)
【7】Ann Rheum Dis:系统性红斑狼疮中使用B细胞生物标记物预测和管理利妥昔单抗无应答
这项研究旨在探讨系统性红斑狼疮(SLE)中利妥昔单抗原发性和继发性无应答的相关因素,并评估继发性非减轻无应答者(2NDNR)的管理。
对 125例利妥昔单抗治疗12年以上的SLE患者进行前瞻性研究。使用高灵敏度流式细胞仪测量B细胞亚群。2NDNR患者,由输液反应和缺陷性减轻定义,使用奥瑞珠单抗或奥法木单抗治疗。
117例患者有可供评估的数据。在周期1(C1)中,96/117(82%)达到了BILAG应答。在多变量分析中,年龄较轻,6周时B细胞减少增加主要应答的几率。完全减轻可由正常补体和较低的前利妥昔单抗成浆细胞预测,并与利妥昔单抗后严重感染的增加无关。77例(72例有数据)C1应答者在临床复发时再治疗。其中61/72(85%)在第2周期(C2)有应答。在11个C2无应答者中,9例符合2NDNR标准,并检测到抗利妥昔单抗抗体阳性。缺乏伴随的免疫抑制剂和更高的前利妥昔单抗成浆细胞可以预测2NDNR。5例转为使用奥瑞珠单抗或奥法木单抗治疗,并全部减轻和应答。(文章详见——Ann Rheum Dis:系统性红斑狼疮中使用B细胞生物标记物预测和管理利妥昔单抗无应答)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#系统性#
116
#研究进展#
101
#狼疮#
125
#红斑#
97
感谢对系统性红班狼疮最新研究会综,学习了。
115
不错的,学习了,谢谢分享!
119