Cell Stem Cell :你对鼓膜了解多少?CELL子刊揭示角质形成细胞是如何维持鼓膜稳态的
2020-11-26 张佳兴 生物探索
鼓膜位于外耳道底,将外耳与中耳分隔开,也承担着声音传递的功能。它将声音从外耳道传导到听骨链,再由听骨链传递到内耳,在内耳转化为神经信号。
鼓膜位于外耳道底,将外耳与中耳分隔开,也承担着声音传递的功能。它将声音从外耳道传导到听骨链,再由听骨链传递到内耳,在内耳转化为神经信号。鼓膜上皮与身体其它部位的表皮类似,但是,由于它位于外耳道盲端,还需要具备清除外耳道的细胞碎片、异物的功能。
鼓膜病变十分常见,如穿孔、收缩、胆脂瘤、鼓室硬化、大疱性鼓膜炎和角化闭塞症等,可导致听力下降、慢性感染、眩晕,严重者可导致脑膜炎或死亡。但人们对于它的了解还远远不够。
近日,国际学术期刊《Cell-Stem-Cell》在线发表了美国加州大学旧金山分校Aaron D. Tward团队名为“A Hierarchy of Proliferative and Migratory Keratinocytes Maintains the Tympanic Membrane”的研究成果,阐明了鼓膜角质形成细胞的增殖、迁移和克隆动态,揭示了其对鼓膜维持的贡献。
研究人员使用单细胞RNA测序、谱系追踪、全器官外植体和活细胞成像技术对鼓膜进行了研究,发现与其它部位的表皮相比,鼓膜呈具有离散的增生区以及多个角质形成细胞群的3D结构。鼓膜干细胞散在分布于鼓膜,并产生长寿命的克隆和定型祖细胞(CP)。
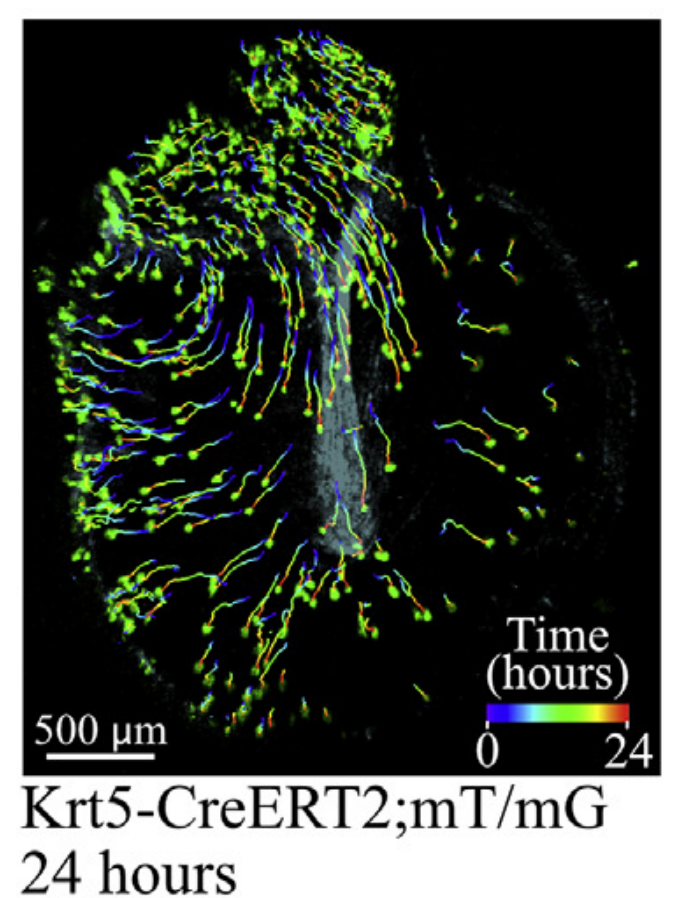
鼓膜活细胞成像
通过活细胞成像技术,研究人员阐明了鼓膜角质形成细胞在鼓膜上由上至下迁移的行为模式,并且发现,这种迁移与细胞增殖具有联系。而谱系示踪描述了鼓膜角质形成细胞的克隆结构,CP在锤骨周围增殖,从紧张部向外迁移。
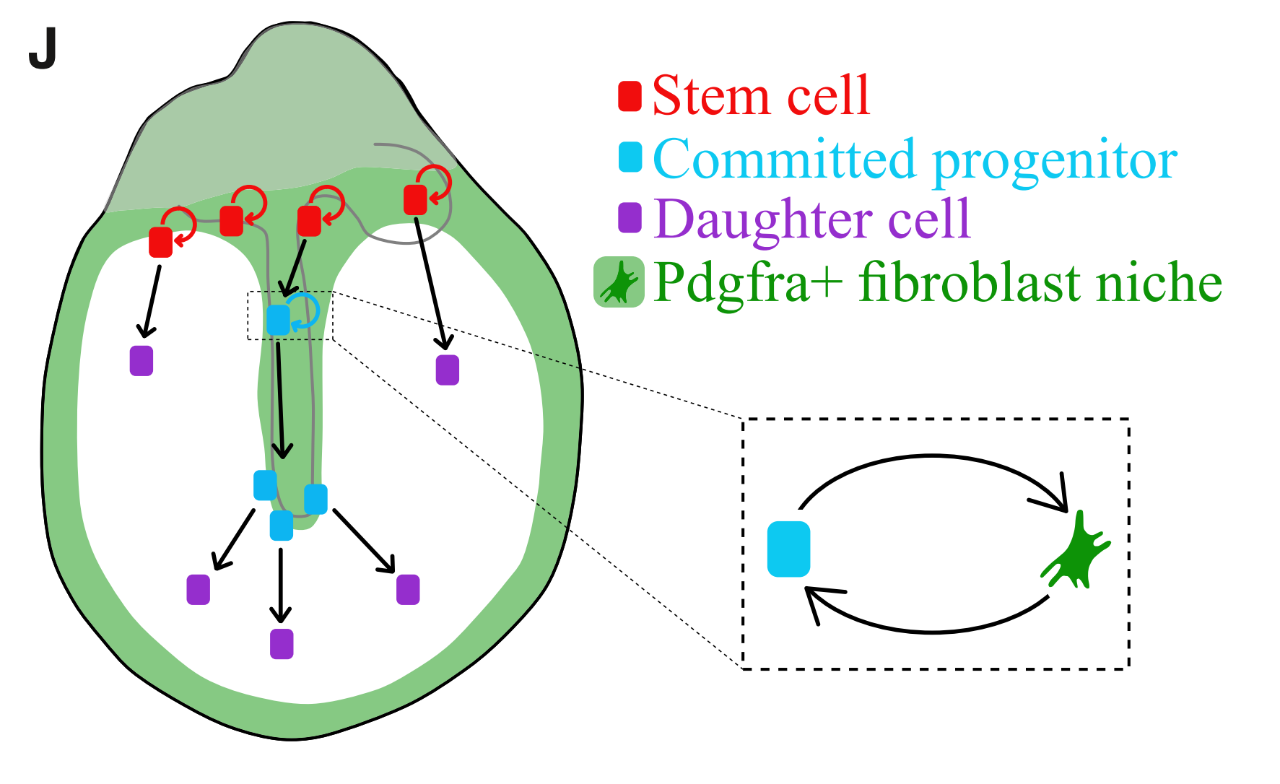
细胞周转示意图
这种增殖模式表明,局部存在促进角质形成细胞周转的信号。研究人员通过筛选发现成纤维细胞中的Pdgfra信号传导支持小鼠和人类TM角质形成细胞的周转。因此,Fgf可能是成纤维细胞到角质形成细胞的信号转导轴的组成部分。
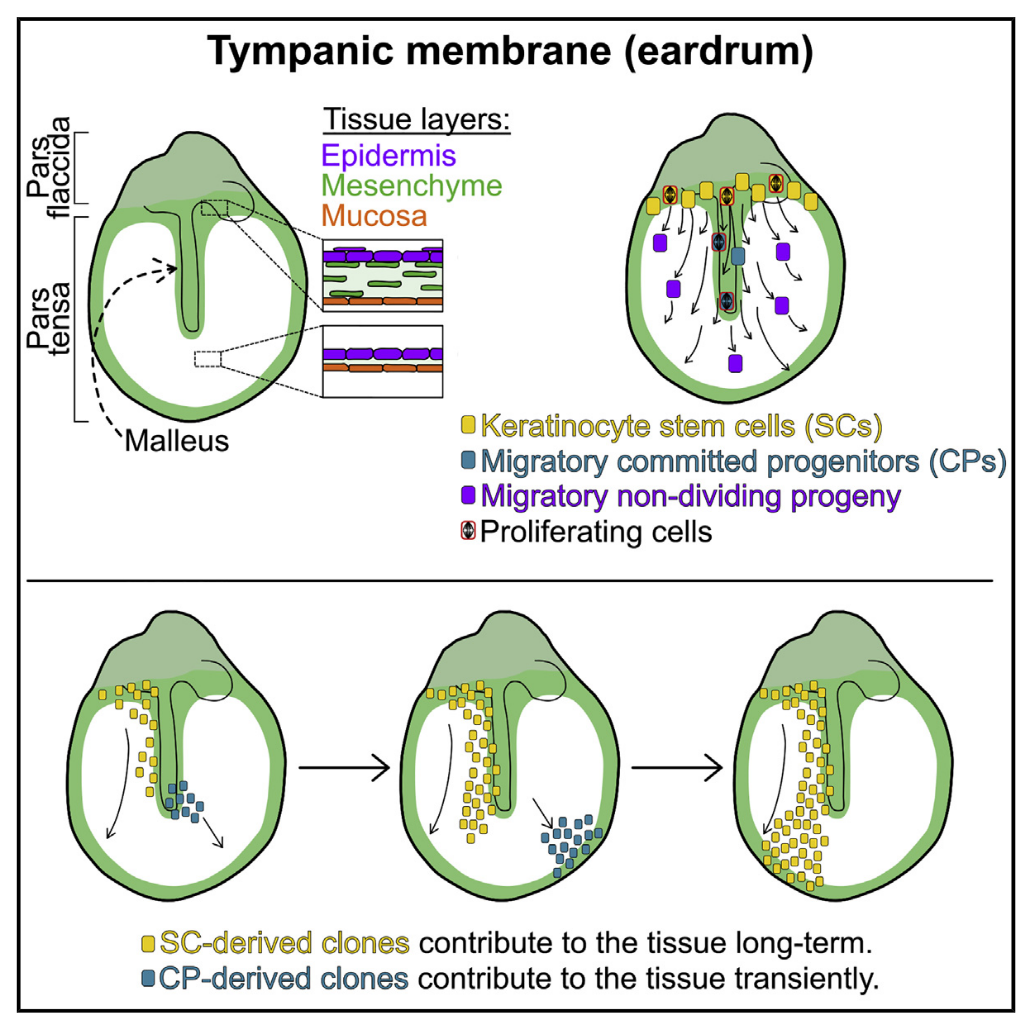
模式图
总的来说,CP克隆倾向于侧向迁移,其增殖能力得到Pdgfra +成纤维细胞的调控产生迁移。此研究揭示了在稳态过程中鼓膜角质形成细胞的增殖、迁移和克隆动态,为理解鼓膜疾病和建模角质形成细胞生物学奠定了基础。
原始出处:
Stacey M Frumm, Shengyang Kevin Yu, Joseph Chang,et al.A Hierarchy of Proliferative and Migratory Keratinocytes Maintains the Tympanic Membrane.Cell Stem Cell. 2020 Nov 5;S1934-5909(20)30500-2. doi: 10.1016/j.stem.2020.10.006.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#stem cell#
126
#稳态#
67
#Cell#
61
#CEL#
54
#STEM#
78