稳定型盔甲样慢性硬膜下血肿1例
2018-10-15 宋熙文 江敦清 方曙平 中国临床神经外科杂志
慢性硬膜下血肿(chronic subdural hematoma,CSDH)发病机制目前尚未明确,血肿常不断进展,很难自愈,需要临床干预;病程常在3个月内,超过1年者少见,有文献报道长达34年。本文报道1例病程超过50年稳定型盔甲样CSDH。
慢性硬膜下血肿(chronic subdural hematoma,CSDH)发病机制目前尚未明确,血肿常不断进展,很难自愈,需要临床干预;病程常在3个月内,超过1年者少见,有文献报道长达34年。本文报道1例病程超过50年稳定型盔甲样CSDH。
1. 病例资料
男,56岁,因头部外伤2 h入院。自述出生时“难产”,婴幼儿时曾患“脊髓灰质炎”,经治疗后遗留右侧肢体残疾。入院时体格检查:GCS评分15分,头颅无畸形,右额部皮肤挫伤,颅神经未见明显异常体征;右侧上、下肢肌肉萎缩,肌力4级;左侧肢体肌力、肌张力正常;双侧Babinski征阴性。头颅CT平扫见左侧额颞顶枕稍低密度新月形病灶(图1A~D)。增强扫描病灶未见强化(图1E~H)。未予特殊治疗,随访观察。
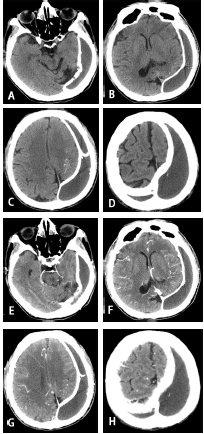
图1 稳定型盔甲样慢性硬膜下血肿CTA~D. CT 平扫,左侧额颞顶枕CSDH;包膜完全钙化;左侧侧脑室及脑实质轻度受压;左侧顶叶区可见沙粒状钙化灶;左侧大脑半球发育不良;E~H.CT 增强扫描示脑血管分布正常,血肿及包膜未见强化
2. 讨论
病人出生时有产伤,婴幼儿期发病,右侧肢体残疾不是脊髓灰质炎后遗症,而是受当时医疗条件所限,为CSDH误诊。1966年,Birkner等对钙化CSDH描述为“大脑由广泛的钙化壳所围绕,类似于盔甲心,称为盔甲脑”。本文病例特点:病程长,达50余年,逐渐形成“盔甲样血肿”;血肿形成到一定量后达稳定状态,出血停止;血肿量大,甚至累及对侧,但脑受压不重;包膜较厚,在6~8 mm,且完全钙化;血肿机化、局部钙化;血肿周围脑组织部分钙化;盔甲样血肿明显影响脑发育,并遗留永久神经功能缺损。
CSDH发病机制仍未明确,多数有头部外伤史。产伤、被虐待、震荡伤是新生儿及婴幼儿CSDH的重要病因。关于CSDH扩大的机制,最早有“渗透压梯度及半透膜学说”,最近的“血肿外膜血管形成、再出血”学说越来越被临床接受。根据“血肿外膜血管形成、再出血”学说,本文病例出生时产伤形成硬膜下血肿,含纤维素的血凝块引起局部非特异性炎症反应,在炎症细胞因子的作用下,血肿包膜不断形成,外膜含丰富新生不成熟毛细血管易出血,再加上局部纤溶亢进而导致不断进展的CSDH。随着包膜内压力不断增高,最终出血停止,包膜局部血管闭塞。随着时间延长,血肿及包膜逐渐机化、钙化,形成少见的稳定型、以血肿及包膜机化伴钙盐沉积为病理改变的盔甲样CSDH。
原始出处:
宋熙文,江敦清,方曙平,李代江,贺英,郭智霖.稳定型盔甲样慢性硬膜下血肿1例[J].中国临床神经外科杂志,2017(12):864.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#硬膜下#
79
#盔甲样#
69
#稳定型#
76
#慢性硬膜下血肿#
90
#血肿#
56
#硬膜下血肿#
64
学习了
104