Blood:用Ravulizumab替代依库丽单抗治疗PNH疗效不变
2018-12-06 MedSci MedSci原创
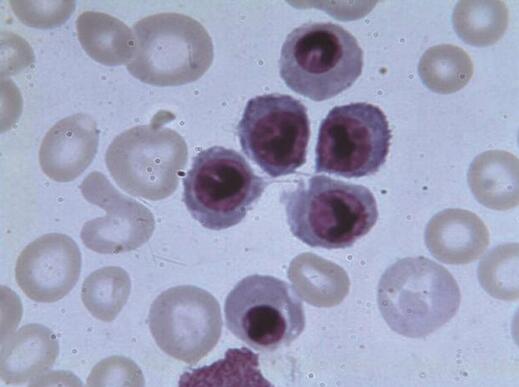
Ravulizumab,是一种新的补体C5抑制剂,用于未进行过补体抑制剂治疗的阵发性夜间睡眠性血红蛋白尿(PNH)患者,每8周给药一次,效果不次于每2周用一次依库丽单抗。现Austin G. Kulasekararaj等人对ravulizumab相比依库丽单抗应用于临床稳定的PNH患者的非劣效性进行评估。研究人员开展一3期的开放性的多中心研究,195位应用依库丽单抗(900mg/2周)超过6个月的
研究人员开展一3期的开放性的多中心研究,195位应用依库丽单抗(900mg/2周)超过6个月的PNH患者被随机(1:1)分至ravulizumab组(97人)或依库丽单抗组(98人,继续用依库丽单抗治疗)。主要结点是从起始到第183天时乳酸脱氢酶(LDH)的变化比例。次要结点包括突破性溶血的患者比例、慢性病治疗功能评估(FACIT)-疲劳评分的变化、输血减少和血红蛋白稳定。
191位患者完成183天的治疗,ravulizumab治疗的效果不比依库丽单抗差(所有p<0.0006),包括LDH的变化比例(差异9.21%[95% CI -0.42~18.84],p=0.058)、突破性溶血(5.1[95% CI -8.89~18.99])、FACIT-疲劳评分(1.47[95% CI -0.21~3.15])、输血减少(5.5[95% CI -4.27~15.68])和血红蛋白稳定(1.4[95% CI -10.41~13.31])。最常见的副反应是头痛(ravulizumab 25.8% vs 依库丽单抗 17.3%)。无脑膜炎球菌感染或因不良事件而停药。
总而言之,PNH患者,从每2周用一次依库丽单抗转为每8周用一次ravulizumab,效果不减,安全性佳。
Austin G. Kulasekararaj,et al. Ravulizumab (ALXN1210) vs eculizumab in C5-inhibitor-experienced adult patients with PNH: the 302 study. Blood 2018 :blood-2018-09-876805; doi: https://doi.org/10.1182/blood-2018-09-876805
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#mAb#
36
#依库丽单抗#
47
#ravulizumab#
65
#PNH#
0
谢谢梅斯提供这么好的信息,学到很多
56
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
64