Clin Cancer Res:复旦肿瘤晚期免疫调节型三阴性乳腺癌(TNBC)新疗法,有效率高达95.8%
2022-03-11 yd2015 MedSci原创
研究表明,法米替尼+卡瑞利珠单抗+白蛋白紫杉醇三联方案治疗晚期免疫调节型TNBC疗效显著,安全性好。
近期,Clin Cancer Res杂志上发表了一项II期临床研究成果(FUTURE-C-Plus),该研究是复旦大学肿瘤医院邵志敏教授牵头的,主要是评估在晚期免疫调节型三阴性乳腺癌(TNBC)中使用Famitinib(法米替尼) + camrelizumab(卡瑞利珠单抗)+白蛋白紫杉醇三联方案治疗的疗效和安全性。

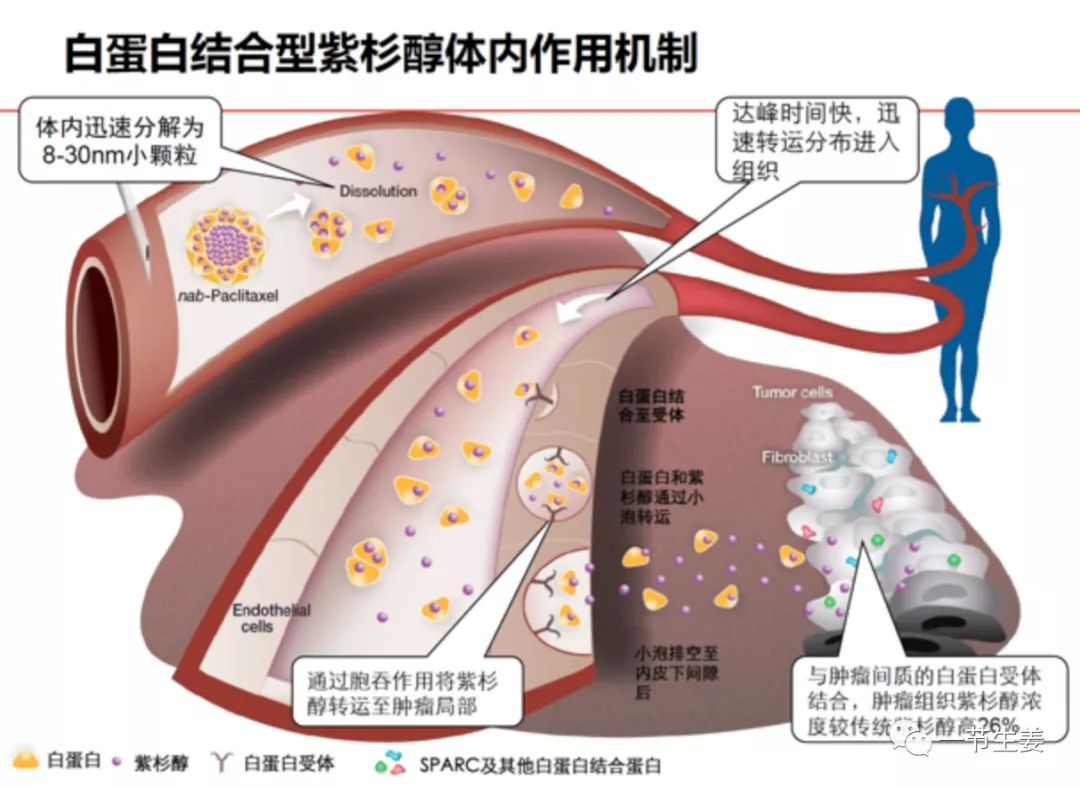
这是一项开放标签、单臂、II期研究,纳入既往未治疗的晚期免疫调节性TNBC患者(CD8 免疫组化染色≧10%)。符合条件的患者在第1-28天给予口服法米替尼20 mg,第1和15天静脉给予卡瑞利珠单抗200 mg,第1、8和15天静脉给予白蛋白紫杉醇100 mg/m2, 每4周为一周期。主要终点为客观缓解率(ORR)。次要终点是无进展生存期(PFS)、总生存期(OS)、缓解期(DOR)、安全性和探索性生物标志物。
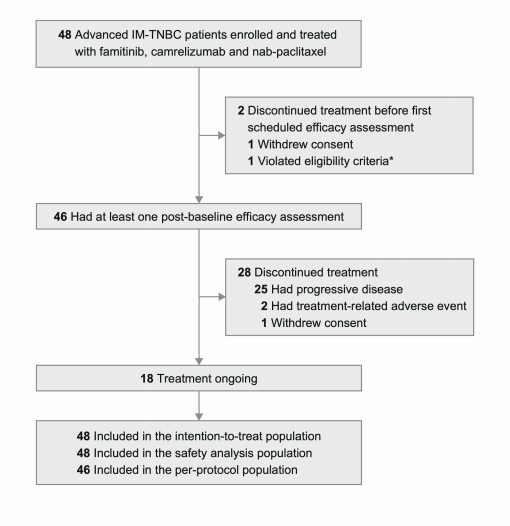
2019年10月-2020年10月,本研究筛选了122例患者,其中48例(39.3%)为确定的CD8阳性(CD8≧10%)。这48例患者入选并接受治疗。所有患者均纳入ITT和安全性分析人群。最终46例患者纳入PP人群分析。截至2021年10月12日数据截止时,中位随访时间为17.0个月(范围8.7-24.3),18名(37.5%)患者仍在接受治疗。患者的中位年龄为50岁(范围25-70岁);23例(47.9%)患者转移部位超过3处,肺转移24例(50.0%),肝转移10例(20.8%)。
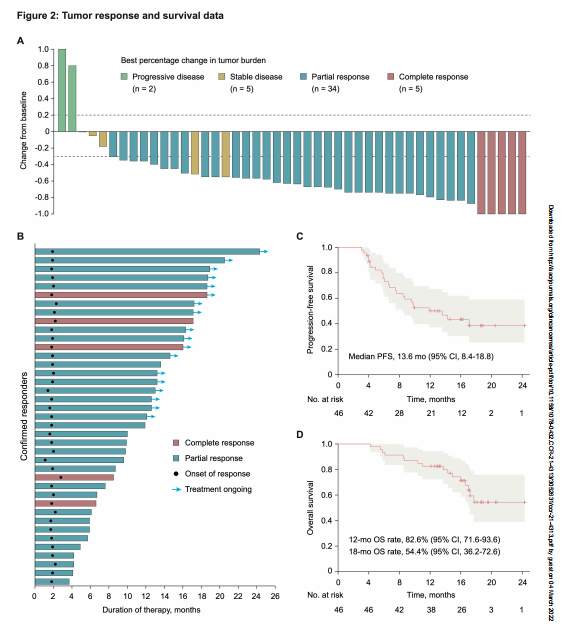
ITT人群中,确认ORR为81.3% (95% CI, 70.2 ~ 92.3),完全缓解5例,部分缓解34例。中位治疗至应答时间为1.9个月(95% CI, 1.8-2.0)。在39例应答患者中,中位DOR为14.9个月(95% CI, NE-NE),其中18(46.2%)例应答患者仍在应答中。DCR为95.8%(46/48)。
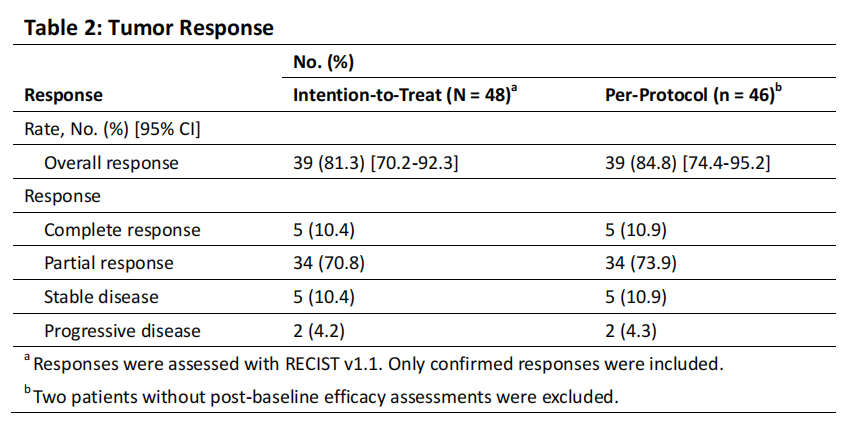
中位无进展生存期为13.6个月(95% CI, 8.4-18.8),中位OS未达到(95% CI, NE-NE);12个月时的OS率为82.6%(71.6-93.6),18个月时为54.4%(36.2%-72.6%)。
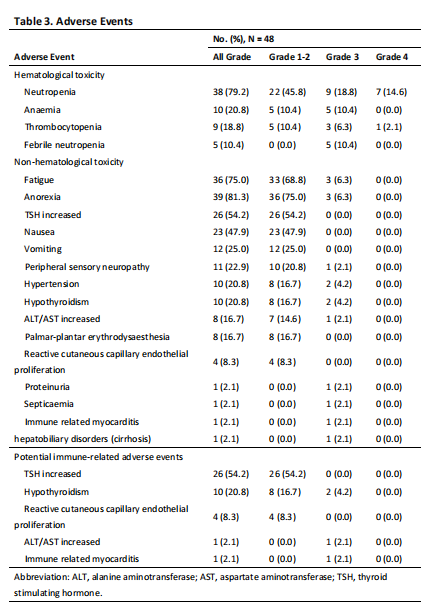
大多数病人(96% [n = 46])至少有一个治疗相关的不良事件(TRAE)。3或4级TRAEs发生在24例(50.0%)患者,最常见的是中性粒细胞减少(33.3% (n = 16))、贫血(10.4% (n = 5))、发热性中性粒细胞减少(10.4% (n = 5))、血小板减少(8.3% (n = 4)),疲劳(6.3% [n = 3])和厌食症(6.3% [n = 3])。3级周围感觉神经病变(2.1%)被认为与紫杉烷相关,并且已知是累积性的。2例(4.2%)患者出现严重TRAE, 1例(2.1%)为3级败血症,1例(2.1%)为3级免疫相关心肌炎。
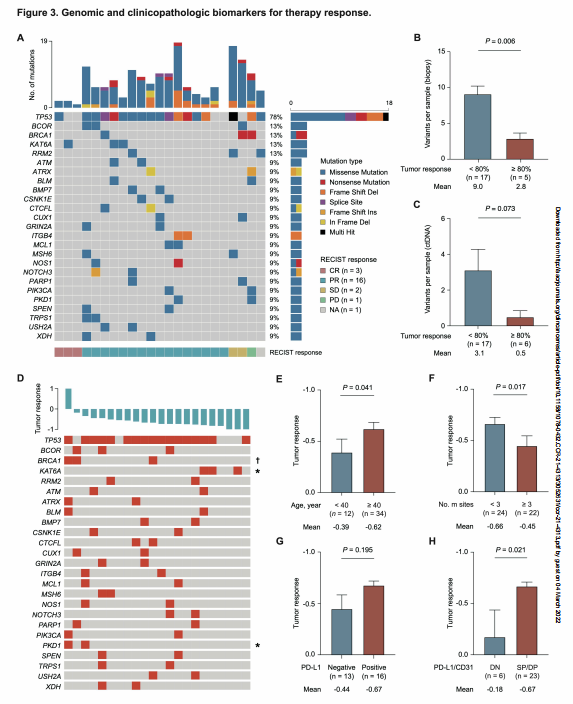
标志物探索发现,晚期免疫调节性TNBC患者中最常见的突变基因为TP53(78%)、BCOR(13%)BRCA1(13%)、KAT6A(13%)和RRM2(13%)。总而言之,KAT6A突变与OR正相关(P = 0.044),而BRCA1 (P = 0.055)和PKD1 (P = 0.034)则表现出相反的趋势。总的来说,PD-L1/CD31双阴性患者对三联治疗方案的反应较差。
综上,研究表明,法米替尼+卡瑞利珠单抗+白蛋白紫杉醇三联方案治疗晚期免疫调节型TNBC疗效显著,安全性好。
原始出处:
Chen L, Jiang YZ, Wu SY, Wu J, Di GH, Liu GY, Yu KD, Fan L, Li JJ, Hou YF, Hu Z, Chen CM, Huang XY, Cao AY, Hu X, Zhao S, Ma XY, Xu Y, Sun XJ, Chai WJ, Guo X, Chen X, Xu Y, Zhu XY, Zou JJ, Yang WT, Wang ZH, Shao ZM. Famitinib with camrelizumab and nab-paclitaxel for advanced immunomodulatory triple-negative breast cancer (FUTURE-C-PLUS): an open-label, single-arm, phase 2 trial. Clin Cancer Res. 2022 Mar 3:clincanres.CCR-21-4313-E.2021. doi: 10.1158/1078-0432.CCR-21-4313. Epub ahead of print. PMID: 35247906.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#阴性乳腺癌#
91
#三阴性#
129
#复旦#
69
#新疗法#
108
感谢分享
95