Pediatr Crit Care Med.:中国淮安地区儿童脓毒症现状调查
2014-12-13 MedSci MedSci原创译
脓毒症是儿童主要的疾病负担,发展中国家脓毒症的分布具有地区性,疾病结局更严重并且发病率逐年升高。严重脓毒症与休克、多器官功能障碍和死亡密切相关,ICU病房内的脓毒症的患病率和死亡率尤其高。为了研究中国淮安地区医院内儿童脓毒症的患病率、治疗和疾病结局,王医生等根据江苏省淮安地区医院信息网络的数据,研究了该地区脓毒症患儿的患病情况。该研究发表在近日的Pediatric Critical Care Me
脓毒症是儿童主要的疾病负担,发展中国家脓毒症的分布具有地区性,疾病结局更严重并且发病率逐年升高。严重脓毒症与休克、多器官功能障碍和死亡密切相关,ICU病房内的脓毒症的患病率和死亡率尤其高。
为了研究中国淮安地区医院内儿童脓毒症的患病率、治疗和疾病结局,王医生等根据江苏省淮安地区医院信息网络的数据,研究了该地区脓毒症患儿的患病情况。该研究发表在近日的Pediatric Critical Care Medicine杂志上。
该研究涉及的淮安地区11个市级、县级医院,共覆盖了843000名儿童的医疗服务。
研究最终纳入了27836名儿童,年龄从28天至15岁不等。共有1530名儿童符合2005年国际共识的脓毒症诊断标准。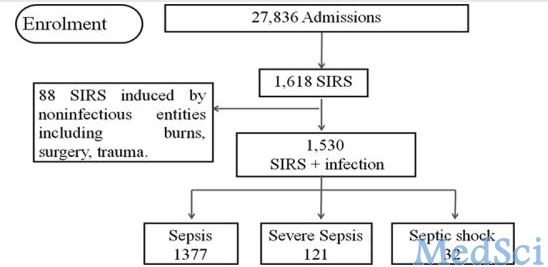
图1 患儿分组情况
研究发现,每万名儿童中就有181名儿童患脓毒症,80%为小于5岁患儿,10%患有严重脓毒症或脓毒性休克。脓毒症的总体死亡率为5.3%,严重脓毒症或脓毒性休克的儿童总体死亡率为34.6%。不同方法各有不同,有的病例甚至不符合国际指南,包括抗生素、糖皮质激素、血管活性药和正性肌力药和的不合理应用。
该研究首次依据地区医院网络研究了中国地区儿童脓毒症的发病率和疾病结局。根据次级医院治疗混乱的现象,作者指出,急需加强乡镇医院的医疗建设,以提高资源匮乏地区的医疗水平。
原始出处:
Wang, Y., et al., An epidemiologic survey of pediatric sepsis in regional hospitals in china*. Pediatr Crit Care Med, 2014. 15(9): p. 814-20.
本文是MedSci原创编译整理,欢迎转载! 转载请注明来源并附原文链接。谢谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








数据庞大
127
#DIA#
47
统计数据好庞大
112
#PE#
40
#Med#
54