Diabetologia:GIP(3-30)NH2是一种有效的GIP受体拮抗剂?
2018-04-24 MedSci MedSci原创
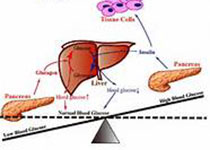
近日,国际杂志 《Diabetologia》上在线发表一项关于GIP(3-30)NH2是在人类中一种有效的GIP受体拮抗剂的随机,双盲,安慰剂对照,交叉研究。 葡萄糖依赖型胰岛素多肽(GIP)是一种肠内内分泌K细胞分泌的内分泌激素,尽管具有一定的治疗效果,但关于人类GIP生理学尚不清楚。通过合适的GIP受体拮抗剂可促进该领域的进展。本研究首次对天然存在的GIP(3-30)NH2在体内和体外受
近日,国际杂志 《Diabetologia》上在线发表一项关于GIP(3-30)NH2是在人类中一种有效的GIP受体拮抗剂的随机,双盲,安慰剂对照,交叉研究。 葡萄糖依赖型胰岛素多肽(GIP)是一种肠内内分泌K细胞分泌的内分泌激素,尽管具有一定的治疗效果,但关于人类GIP生理学尚不清楚。通过合适的GIP受体拮抗剂可促进该领域的进展。本研究首次对天然存在的GIP(3-30)NH2在体内和体外受体研究中的拮抗特性开展了研究。 研究人员在瞬时转染的COS-7细胞中,在glucagon样肽1 (GLP-1)、glucagon-like peptide-2 (GLP-2)、胰高血糖素、分泌素和生长激素释放激素(GHRH)受体的同源受体结合和受体激活(cAMP积累)研究中评估GIP(3-30)NH2。临床研究纳入10名健康男性(合格标准:年龄20-30岁,HbA 1c低于6.5%[48 mmol/mol]和空腹血糖[FPG]低于7 mmol/l)。收集来自肘静脉套管的血浆和血清样品数据。作为主要结果,在高血糖钳夹实验中通过输注GIP(3-30)NH 2(800pmol kg -1 min-1),G
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











求GIP的机制
77
#DIA#
63
#BET#
78
#拮抗剂#
80