JAMA Cardiol:急性冠状动脉综合征患者复杂PCI后采用普拉格雷降级治疗有利无害!
2022-04-25 Nebula MedSci原创
普拉格雷剂量降级治疗不会增加ACS患者的MACE事件风险,而且还会降低出血事件发生率。
通过减少普拉格雷的剂量来降低双抗血小板治疗可改善急性冠脉综合征(ACS)患者随后的净不良临床事件,即在减少出血事件的同时不增加缺血性事件。但是,在接受复杂手术的患者中是否也能观察到类似的好处,目前尚不清楚。
本研究是HOST-REDUCEPOLYTECH-ACS试验(一项随机、开放标签、评判员单盲的多中心试验)的事后分析,旨在探索在接受复杂的经皮冠状动脉介入治疗 (PCI) 的亚组患者中,普拉格雷剂量降级治疗的益处是否得到维持。
受试患者是接受PCI治疗的急性冠脉综合征患者,PCI术后1月时被随机分至普拉格雷剂量降级治疗组(5 mg/天)或常规治疗组(10 mg/天)。复杂PCI的定义是至少具有以下一种特性:植入3个或以上支架,治疗3个或以上病变,PCI分叉,总支架长度>60 mm,左主干PCI或重度钙化。主要终点是一年内缺血性结局的主要不良心血管事件(MACE,包括心血管死亡、非致死性心肌梗死、支架血栓形成及重复血运重建)和BARC 2级及以上的出血事件。
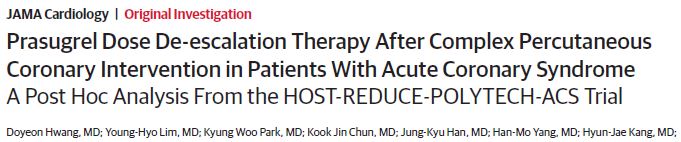
两组患者的MACE和出血事件的发生率
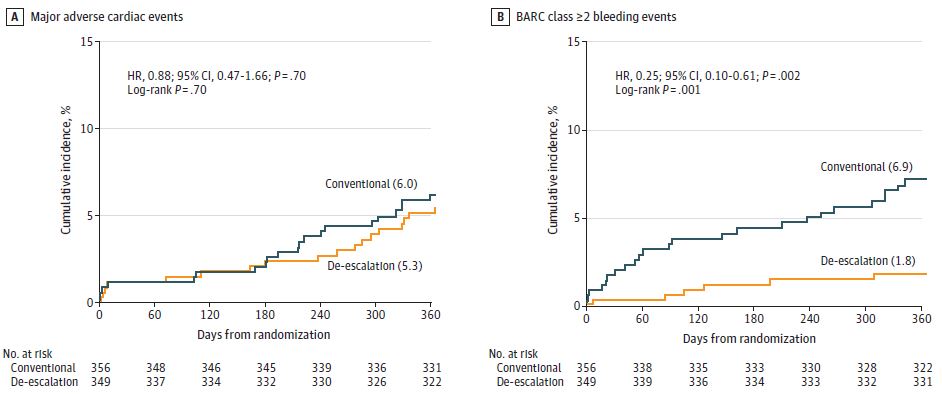
共招募了2271位患者(平均 58.9岁;2024位[89%]男性),其中705位接受了复杂PCI,1566位接受了非复杂PCI。普拉格雷剂量降级治疗并不增加MACE事件风险(复杂PCI和非复杂PCI患者的风险比[HR]分别是0.88[p=0.70]和0.81[p=0.48]),而且还会降低BARC 2级及以上出血事件的发生率(HR 0.25[p=0.02]和0.62[p=0.05])。复杂PCI与更高的缺血性结局发生率相关,但与出血结局发生率无明显相关性。
复杂PCI vs 非复杂PCI 患者的MACE和出血事件的发生率
综上,该研究结果提示,无论PCI复杂与否,与常规治疗相比,普拉格雷剂量降级治疗都不会增加患者一年内缺血性事件结局的风险,而且还可以降低出血事件风险。
原始出处:
Hwang Doyeon,Lim Young-Hyo,Park Kyung Woo et al. Prasugrel Dose De-escalation Therapy After Complex Percutaneous Coronary Intervention in Patients With Acute Coronary Syndrome: A Post Hoc Analysis From the HOST-REDUCE-POLYTECH-ACS Trial.[J] .JAMA Cardiol, 2022, 7: 418-426. https://doi.org/10.1001/jamacardio.2022.0052
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#冠状动脉综合征#
93
#Cardiol#
69
#综合征#
75
学习
77
JAMA上文章都是顶级的,谢谢梅斯及时上新
100