Antimicrob Agents Chemother:碳青霉烯类治疗不动杆菌菌血症:MIC值为多少时获益更多?
2017-09-28 吴星 环球医学
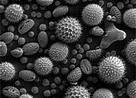
临床和实验室标准协会(CLSI)和欧洲委员会关于抗菌药物的敏感试验(EUCAST)为不动杆菌菌血症提供了不同的碳青霉烯类MIC推荐。此外,中级范畴的临床有效性仍然不确定。2017年8月,发表在《Antimicrob Agents Chemother》的一项研究调查了碳青霉烯类MIC值与不动杆菌菌血症患者的临床结局的相关性。
临床和实验室标准协会(CLSI)和欧洲委员会关于抗菌药物的敏感试验(EUCAST)为不动杆菌菌血症提供了不同的碳青霉烯类MIC推荐。此外,中级范畴的临床有效性仍然不确定。2017年8月,发表在《Antimicrob Agents Chemother》的一项研究调查了碳青霉烯类MIC值与不动杆菌菌血症患者的临床结局的相关性。
设计该研究旨在考察使用碳青霉烯类治疗不动杆菌菌血症患者生存预测的最佳分界点。
研究者在5年时间里,根据最初分离菌株的碳青霉烯类MICs,分析了4个医疗中心224例初始使用碳青霉烯类单药疗法治疗不动杆菌菌血症的成人患者的30天死亡率。
分离菌株中碳青霉烯类MICs≥8 mg/L的患者的30天死亡率大约是分离菌株中碳青霉烯类MICs≤4 mg/L的患者的2倍。根据双变量分析(53.1% [60/113] vs 25.2% [28/111;p<0.001)和时序检验生存分析的差异具有显着性(p<0.001)。分类和回归树分析显示,4 mg/L至8 mg/L MICs之间的差异,并预测相似的差异死亡率(p<0.001)。碳青霉烯类治疗由碳青霉烯类MICs≥8 mg/L引起的不动杆菌菌血症是30天死亡率的一个独立预测因素(比值比,4.218;95%置信区间,2.213~8.039;p<0.001)。
该研究显示,使用碳青霉烯类治疗不动杆菌菌血症的患者,在其分类菌株的碳青霉烯类MICs≤4 mg/L时,可以比MICs≥8 mg/L获得更多的有益结局。
原始出处:
Yang YS, Wang YC, Kuo SC,et al. Multicenter Study of the Relationship between Carbapenem MIC Values and Clinical Outcome of Patients with Acinetobacter Bacteremia. Antimicrob Agents Chemother. 2017 Aug 24;61(9). pii: e00661-17. doi: 10.1128/AAC.00661-17. Print 2017 Sep.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Agent#
27
#碳青霉烯类#
48
#agents#
33
#Micro#
32
#CRO#
26
#菌血症#
27