静脉全麻下宫腔镜子宫肌瘤切除术术中失血性休克复苏成功1例
2020-04-29 黄长飞 郭傲 张璟 中国实验诊断学
患者女性,29岁,55kg。因“经期延长伴经量增多2年”入院,诊断为子宫黏膜下肌瘤,拟全麻下行子宫肌瘤切除术。既往体健,剖宫产术后4年,否认过敏史。入院血常规检查示中度度贫血,其他术前常规检查未见明显
1.临床资料
患者女性,29岁,55kg。因“经期延长伴经量增多2年”入院,诊断为子宫黏膜下肌瘤,拟全麻下行子宫肌瘤切除术。既往体健,剖宫产术后4年,否认过敏史。入院血常规检查示中度度贫血,其他术前常规检查未见明显异常。给予输血等相关术前准备。患者步入术间,给予吸氧,开放右上肢静脉通路。
常规监测:5导联心电图(ECG)、无创袖带血压(BP)、脉搏血氧饱和度(SPO2)、心电图(ECG)、呼气末二氧化碳分压(PetCO2)。入室SPO2 100%,HR 66bpm,BP 118/60mmHg。
麻醉诱导:静脉输注咪达唑仑3mg,丙泊酚80mg,芬太尼0.2mg。麻醉深度合适,生命体征平稳后顺利插入3号喉罩并控制呼吸,气道峰压(P peak)17 cmH2O,Pet-CO2 32mmHg,丙泊酚20ml/h泵注维持麻醉。手术历时20min,术中输液500ml,显性出血量约100ml,手术结束后缩宫素30u+0.9%氯化钠500ml静脉滴注。
手术进行15 min时患者HR95bpm,BP88/50mmHg,SPO2 100%,加快胶体液长源雪安输注,减小丙泊酚用量,给予去甲肾上腺素4μg/ml反复静推,同时再放一条静脉通路。术后10min患者心率逐渐增至140bpm,窦性律齐,SPO2无规则波形显示,数据测不出,无创袖带血压测不出,P peak 17 cmH2O,PetCO2 25mmHg,给予甲氧明2mg静推,甲强龙80mg静推,停用长源雪安改输羟乙基淀粉并将液体速度开至最大,拟行动脉血气分析但未能成功。
触摸颈动脉无搏动,立即开始胸外按压,肾上腺素1mg静推2次,0.2μg/kg·min泵注,去甲肾上腺素50μg/ml反复静推,地塞米松10mg静推,紧急取血,冰帽颅温,紧急行气管内插管,动脉穿刺置管测压和颈内静脉穿刺置管。术后30 min有创血压(IBP)105/72 mmHg,HR123bpm,SPO2 100%,动脉血气:pH 7.42,PaCO2 34 mmol/L,PaO2 249 mmol/L,HCO3-std 23.2mmol/L,血红蛋白47g/L,血糖18.0mmol/L,给予加压输血,纠酸,补钾,补钙,降糖等措施维持内环境稳定,并根据病人血压情况调整血管活性药用量。
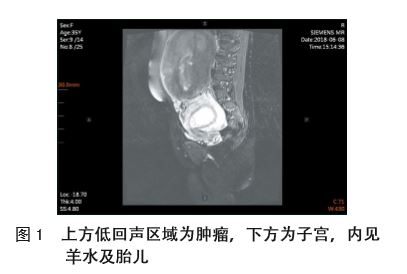
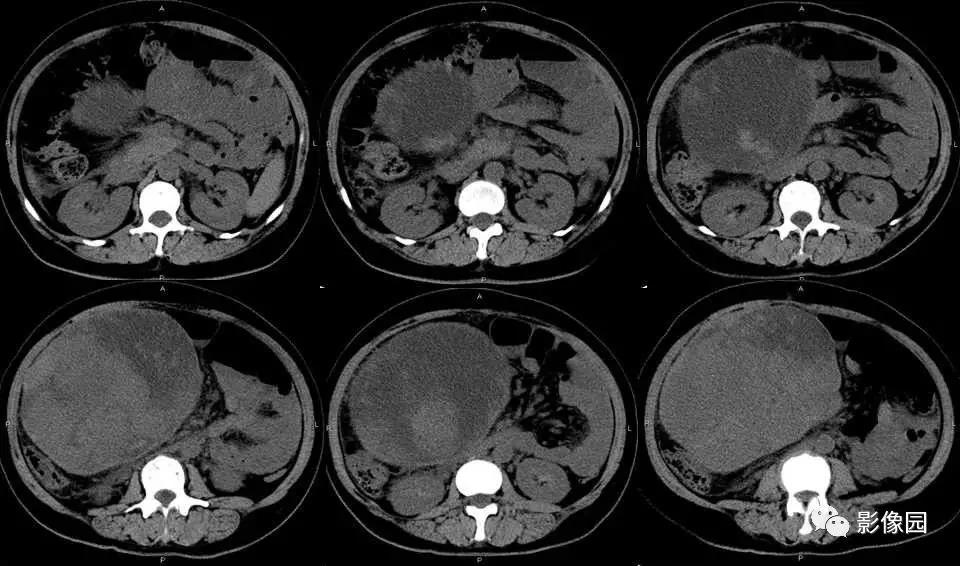
术后35min发现患者腹部稍有膨隆,阴道流血,色鲜红量不多,尿色清。超声检查见腹腔内大量液体,超声引导下腹腔穿刺抽出不凝血,因无法排除膨宫介质(5%葡萄糖)及子宫肌瘤切除后创面渗血由输卵管流入腹腔,贸然开腹后宫腔内压降低有加重出血可能,暂时静滴缩宫素,宫腔填塞,腹部加压控制子宫出血,观察病情变化。
30min后发现患者腹部膨隆进行性增大,挤压子宫,阴道流血约100ml,动脉血气血红蛋白值未测出,血细胞比容(HCT)<15%,此时已输入浓缩红悬3U,血浆370ml,经综合考虑决定行剖腹探查术。给予芬太尼0.1mg,顺阿曲库铵10mg,吸入1%七氟醚,患者生命体征平稳,术中见子宫狭部前壁瘢痕破裂出血,未探及内胀损伤,盆腔内吸出血性液体及血凝块共约4 000ml,行子宫破裂修补术。手术历时1h15min,术中共输注红悬17单位,血浆1 780ml,冷沉淀20单位,输液3 900ml,引出尿液约2 000ml,色清。
术毕持续泵入血管活性药,血压110/70mmHg,心率110bpm,血红蛋白87g/L,血糖10.4mmol/L,患者意识清醒,能配合,自主呼吸,带气管导管送入ICU。次日患者意识清楚,生命体征平稳,引流及切开渗液少,阴道流血少,色暗红,未见其他并发症,拔除气管导管后转入妇科。10日后患者出院。
2.讨论
宫腔镜手术以其安全、有效、简单、微创、体表无痕等优点,在子宫腔内和宫颈疾病的诊断和治疗方面得到极大的发展和推广,宫腔镜手术并发症病例也得到极大积累。宫腔镜手术常见并发症有出血(0.76%-2%),子宫穿孔(0.12%-1.6%),宫颈撕裂(1-11%)和液体超负荷(0.1%-0.2%)。其中子宫穿孔是最常见的并发症,且可继发失血、内脏损伤,甚至危及生命。根据Aubrt A等的前瞻研究,大部分子宫穿孔均能在术中发现,仅有1例(1/2116)未及时发现造成低血容量性休克,经抢救后腹腔镜下子宫穿孔修补术后好转。Lee等也报道了一例宫腔镜手术术中并发子宫穿孔,未及时发现膨宫液流入腹腔造成腹腔间隔室综合征的病例。由于宫腔镜手术需要能量设备、膨宫介质、宫内压力,以及手术空间狭小、不能缝合等特点,使其并发症不同于传统手术。本文从高危宫腔手术的识别、宫腔镜手术麻醉方法的选择、宫腔镜手术并发症的预防识别和处理三方面展开论述。
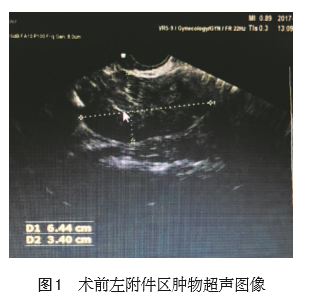
术前除了常规术前询问病史和术前检查外,麻醉医师还应了解患者是否有宫腔粘连、瘢痕子宫、宫腔狭窄、子宫过度前倾后屈萎缩等宫腔镜手术并发症高危因素,以及占位性病变与子宫和盆腔的位置关系,预计手术创面的大小和手术时长,结合术者的经验等因素综合评估患者宫腔镜手术并发症风险,并制定相应麻醉计划。B超监测引导下实施宫腔镜手术,可动态观察子宫腔、子宫肌壁与病灶的关系及手术操作全过程,并且具有简便、经济、安全、有效等优点,成为高危宫腔镜手术的首选监测方法。
患者有剖宫产手术史,属瘢痕子宫,患者术前宫腔出血尚未控制,影响宫腔镜手术视野,延长手术时间,增加子宫穿孔可能,应按高危宫腔镜处理,建议使用术中超声监测。可供选择的麻醉方法有椎管内麻醉和全身麻醉。Motti Goldenberg等报道,与硬膜外麻醉相比全麻下宫腔镜手术时间无差别,而膨宫液的吸收却明显少于硬膜外麻醉病人。膨宫液的过度吸收可影响患者的血糖、血钠和导致液体超负荷的发生。这些病人中虽无液体超负荷的报告,但对于心肺肾功能差,液体负荷敏感的病人和有手术并发症高危因素的复杂长时间宫腔镜手术,选择全身麻醉下宫腔镜手术更有优势。
患者术前有潜在循环血量不足,麻醉开始前应积极补液,备血管活性药备血,麻醉方式以全麻为宜。宫腔镜手术术中管理应特别关注其特有并发症如子宫穿孔(Uterine Perforation)、出血(Hemorrhage)、液体超负荷(Fluid Overload)、静脉空气栓塞(Air Embolism)等。
①此例患者,当心率增快,血压逐渐降低至测不出,指脉氧无规律波形的过程中,首先考虑循环血量不足引起的心率快、血压低,但术中显性出血约100ml,尽管术前患者存在循环血量不足,经过补液治疗,尚不足以解释失血性休克,但应想到子宫穿孔造成的腹腔内出血。
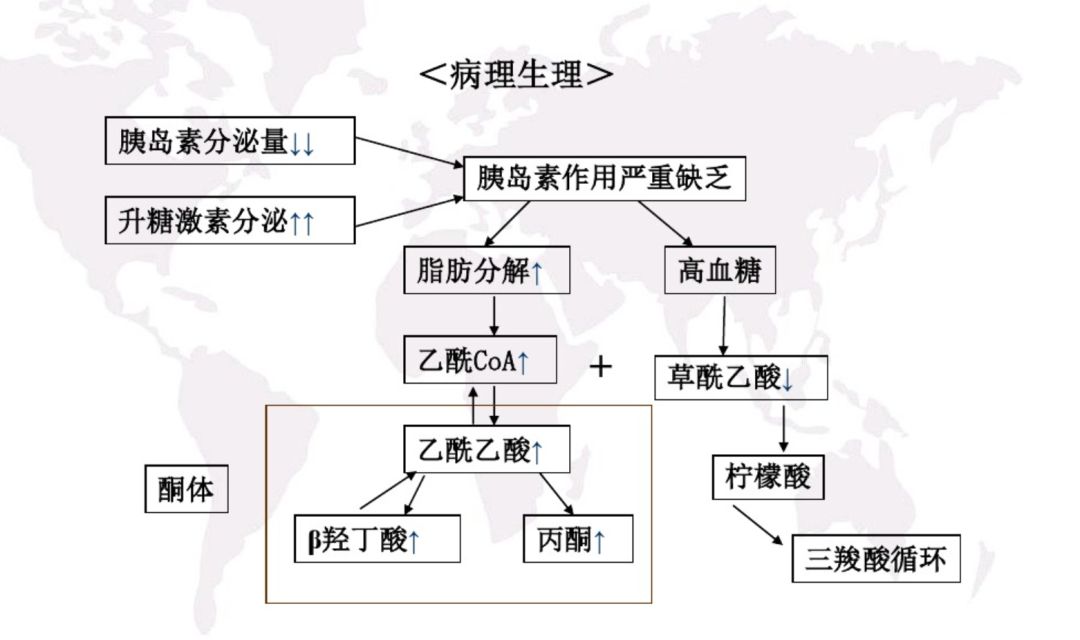
②液体超负荷和高渗高血糖昏迷临床表现为肺水肿、急性左心衰、脑水肿、电解质紊乱的症状和体征。液体超负荷的高危因素有使用低渗或非电解质液膨宫、膨宫压力过大(大于100mmHg)、膨宫时间过长(大于1h)、子宫肌层大面积血管暴露。本例患者为年轻女性,心功能良好,手术时长较短,暂不考虑,可通过术中血气分析和计算膨宫液出入量的方法确诊。
③全麻宫腔镜手术中气体栓塞者会有呼气末二氧化碳分压(PetCO2)突然下降(大于2mmHg)、低血容量无法解释的持续性低血压、心动过速、心动过缓、室性早搏、S-T段改变甚至停搏,但几乎所有气体栓塞患者都有血氧饱和度(SpO2)下降。此例患者虽有PetCO2下降,持续性低血压及心动过速,但SpO2一直是100%,且心动过速是窦性心律,术中未看到早搏,因此可排除气体栓塞的诊断。可通过术中经食管超声心动图、心前区多普勒超声确诊,心前区听诊闻及水轮因也支持诊断。
④术中过敏性休克临床表现多样,特异性不强。本例患者否认过敏史,术中虽有低血压和心动过速,但没有气道痉挛和全身皮肤红疹等临床表现,术中过敏性休克暂不作为首先考虑,待找到更合理的原因后再排除此诊断。根据上述分析,目前仍考虑失血性休克,血气分析见血红蛋白持续降低,腹部膨隆,超声见腹腔内大量液体,腹腔穿刺抽出不凝血证实确有腹腔内出血。腹腔内血液可能来源于腹腔镜手术术中子宫穿孔,也可能源于术中膨宫液由输卵管流入腹腔。液体由输卵管流入腹腔不能解释患者严重循环系统表现和持续低血红蛋白。
根据Janka PS的研究,绝经前女性宫腔镜手术中膨宫液由输卵管流入腹腔的速率为1.5±0.2ml/min,这样的渗液时不会造成上述表现的,可基本肯定为宫腔镜术中子宫穿孔,随后的开腹手术证实了这一点。本例患者生命体征不稳,已危及生命,出血部位不定,显然应立即开腹探查止血。宫腔镜手术时间短创伤小,但宫腔镜手术有它独特危险因素和术中并发症。患者围术期安全需要麻醉医师们术中保持高度警惕,同时也需要和手术医师术中密切配合。
原始出处:
黄长飞,郭傲,张璟,石宏宇,刘铁成.静脉全麻下宫腔镜子宫肌瘤切除术术中失血性休克复苏成功1例的报道[J].中国实验诊断学,2019,23(05):896-898.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#失血性#
65
#失血性休克#
112
#子宫肌瘤切除术#
71
#切除术#
76
#静脉#
82
#复苏#
0
#宫腔镜#
89
#全麻#
80
#失血#
69