Oncologist:真实世界数据表明转移性ALK重排非小细胞肺癌(NSCLC)患者三线使用ALK抑制剂和化疗治疗无显著差异
2022-02-23 yd2015 MedSci原创
研究表明,转移性ALK重排非小细胞肺癌(NSCLC)患者中三线使用ALK抑制剂和化疗治疗无显著差异。
ALK抑制剂(ALKi)是转移性ALK重排非小细胞肺癌(NSCLC)一线和二线治疗的标准治疗方案。近期,来自以色列团队开展了一项多中心真实世界研究,目的是在转移性ALK重排非小细胞肺癌(NSCLC)患者中三线使用ALKi对比化疗治疗的疗效。相关结果发表在Oncologist杂志上。

研究纳入170例患者,约一半为男性,中位年龄为60岁(范围20-89岁)。49例(28.8%)患者在诊断时出现脑转移,38例(22.3%)患者在使用ALKi时诊断为脑转移。
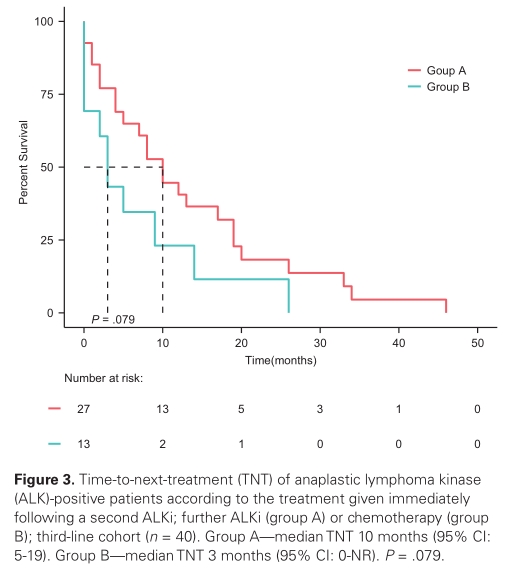
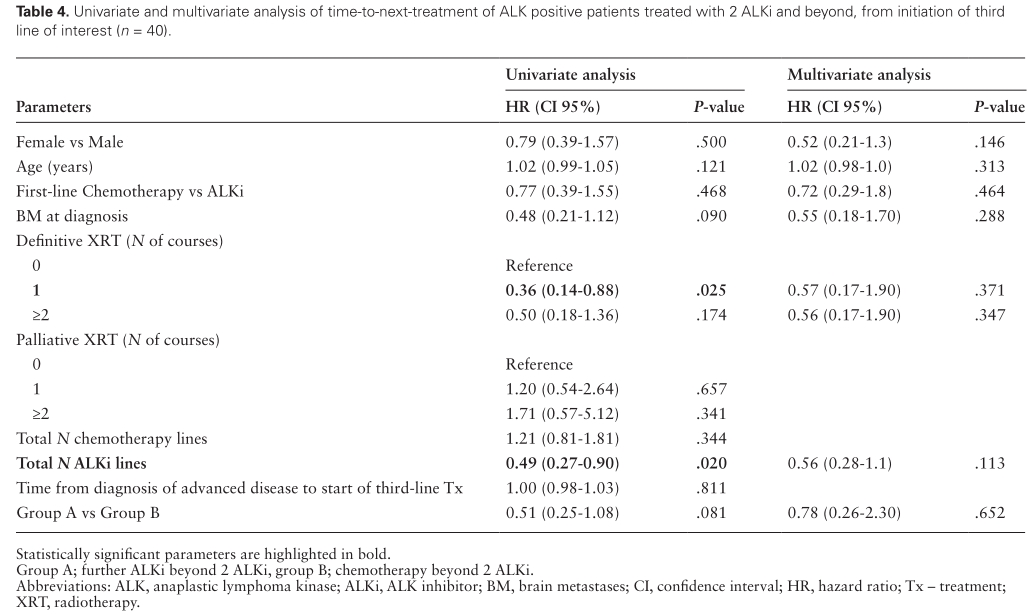
在三线治疗队列中,27例患者接受ALKi治疗(A组),13例(32.5%)患者接受化疗(B组)。A组三线队列中使用的ALKi最常见的是alectininib(55.6%),其次是brigatinib(33.3%),少数使用crizotinib(3.7%)和lorlatinib(7.4%)。B组治疗方案包括铂-培美曲塞(8例,62%)、单药培美曲塞(3例,23%)、单药长春瑞滨(1例,7.5%)和单药pembrolizumab(1例,7.5%)。
中位随访时间为41个月(95% CI: 32-55),全队列(n = 170)中有80人(47.1%)死亡。从诊断为晚期疾病开始,整个队列的中位OS为52个月(95% CI: 32-65)。

在整个队列中,与患者较长的OS显著相关的唯一因素是年轻(HR 1.02, 95% CI: 1.01-1.04, P =0.009)和多线的ALKi治疗(HR 0.765;95%CI:0.61-0.95;P =0.024)。

在三线治疗的队列中,25 (62.5%) 例患者死亡, 包括A组中16 (59.3%)例患者, 和B组9(69.2%) 例患者。从三线治疗开始A组的中位OS为27个月(95% CI: 13-NR) ,B组为3个月(95% CI: 3-NR),但是统计学无显著差异(P =0 .12)。从诊断为晚期疾病开始时,A组的中位OS为65个月(95% CI:32-NR),B组为55个月(95% CI:46-NR),统计学同样无显著差异(P = 0.12)。

从第三线治疗开始至下一线治疗的时间(TNT), A组为10个月(95% CI: 5-19), B组为3个月(95% CI: 0-NR, P =0.085)。
综上,研究表明,转移性ALK重排非小细胞肺癌(NSCLC)患者中三线使用ALK抑制剂和化疗治疗无显著差异。
原始出处:
Mor Moskovitz , Elizabeth Dudnik, Sivan Shamai, et al. ALK Inhibitors or Chemotherapy for Third Line in ALK-positive NSCLC? Real-world Data. The Oncologist, 2022, 27, e76–e84. https://doi.org/10.1093/oncolo/oyab005. Advance access publication 28 January 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#抑制剂#
111
#非小细胞#
90
#Oncol#
58
#真实世界#
78
#转移性#
109
#ALK抑制剂#
135
#GIST#
80