LX9211治疗神经性疼痛,即将开展II期临床研究
2021-01-03 Allan MedSci原创
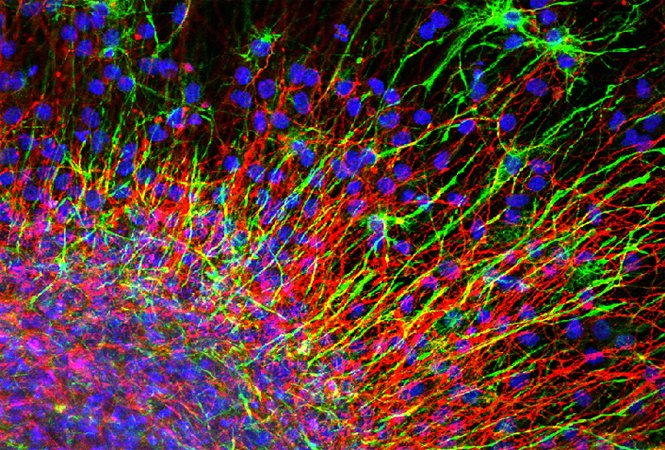
LX9211是一种有效的、口服递送的选择性AAK1小分子抑制剂。制药公司Lexicon将AAK1确定为治疗神经性疼痛的靶点。
传入阻滞性疼痛是由于周围或中枢传入神经的部分或完全异常引起。最常见的是疱疹后神经痛和中枢性疼痛。其具体机制尚不明确,可能与中枢神经系统敏感性上调及疼痛感受区域的扩大和其阈值下降有关。

LX9211是一种有效的、口服递送的选择性AAK1小分子抑制剂。制药公司Lexicon将AAK1确定为治疗神经性疼痛的靶点。LX9211已获得美国食品药品监督管理局(FDA)的“快速通道资格”,用于治疗糖尿病周围神经性疼痛。
Lexicon近日宣布,已经开始LX9211治疗疱疹后神经痛的随机、安慰剂对照、多中心II期临床试验(RELIEF-PHN 1研究)。
Lexicon研发执行副总裁Praveen Tyle博士说:“疱疹患者通常在皮疹清除后几个月至数年内仍会遭受持续的疼痛,目前治疗方法有限。我们相信LX9211有潜力提供疱疹治疗后神经痛的新型治疗方法”。
RELIEF-PHN 1研究旨在评估LX9211在带状疱疹治疗后神经痛中的功效、安全性和药代动力学。该研究将在大约30个临床中心招募大约74名患者。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#II期临床研究#
66
#神经性#
63
#I期临床#
65
#神经性疼痛#
72
#II期临床#
73
好久没来学习了
122
学习了
109