Blood:PET适应性方法用于晚期霍奇金淋巴瘤的局限性和意义——5年随访结果
2019-07-25 MedSci MedSci原创
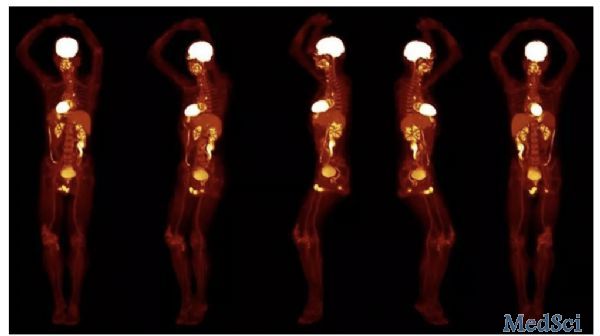
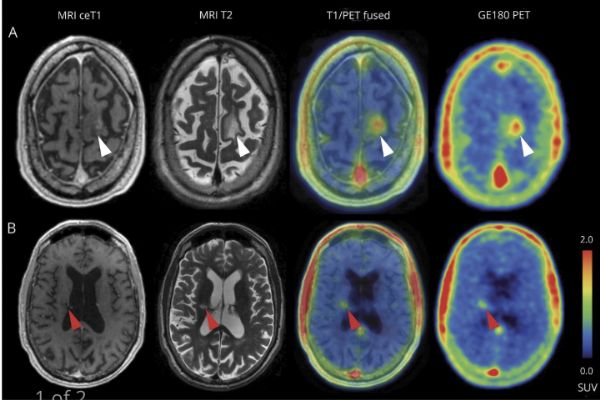
在S0815研究中,晚期霍奇金淋巴瘤(HL)患者在经正电子发射断层扫描(PET)适应性治疗后,2年无进展存活率(PFS)表现良好。患者接受2个周期的阿霉素、博来霉素、长春碱和达卡巴嗪(ABVD)治疗。PET2 (Deauville 评分≤3)完全缓解(CR)的患者继续接受另外4个ABVD疗程治疗。未达到PET2 CR (Deauville评分>3)的患者改用升级的博莱霉素、依托泊苷、阿霉素、环磷酰
约25%的PET2阴性患者会复发,提示一线ABVD疗法具有限制性和较低的PET2阴性预测价值
对于采用eBEACOPP治疗的PET2阳性患者,PFS是有利的,但与较高的第二癌症发生率相关
摘要:
在S0815研究中,晚期霍奇金淋巴瘤(HL)患者在经正电子发射断层扫描(PET)适应性治疗后,2年无进展存活率(PFS)表现良好。患者接受2个周期的阿霉素、博来霉素、长春碱和达卡巴嗪(ABVD)治疗。PET2 (Deauville 评分≤3)完全缓解(CR)的患者继续接受另外4个ABVD疗程治疗。未达到PET2 CR (Deauville评分>3)的患者改用升级的博莱霉素、依托泊苷、阿霉素、环磷酰胺、长春新碱、丙卡嗪和泼尼松(eBEACOPP)治疗6个疗程。
本研究共分析了336例符合条件的患者(其中331例患者进行了PET2复查),随访了5年。82%的患者为PET2阴性,阳性占18%。5年PFS为74% (95%CI:69%-79%)。PET2阴性患者的5年PFS为76% (95%CI:70-81%)。PET2阳性患者的为66% (95% CI:52-76%)。所有患者的5年总存活率(OS)为94% (95%CI:91%-96%)。
在接受eBEACOPP治疗的患者中,有7例(14%)报告发生第二癌症,而接受ABVD治疗的患者中有6例(2%)报告发生第二癌症(P=0.001)。参与S0816试验的HL患者的长期OS仍然很高。但近25%的PET2阴性患者复发,提示一线ABVD治疗和PET2的阴性预测意义均具有局限性。接受eBEACOPP治疗的PET2阳性患者的PFS较好,但与既往对照相比,PFS与第二恶性肿瘤的高发生率相关。
总而言之,本研究结果强调了长期随访的重要性,以及对晚期HL患者采取更有效、毒性更小的治疗方法的必要性。
Deborah M Stephens, et al.Five-Year Follow-up of SWOG S0816: Limitations and Values of a PET-Adapted Approach for Stage III/IV Hodgkin Lymphoma.Blood 2019 :blood.2019000719; doi: https://doi.org/10.1182/blood.2019000719
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
61
#随访结果#
71
#晚期霍奇金淋巴瘤#
95
#5年随访#
84
#局限性#
94
#PET#
65
#适应性#
70