Science丨曹雪涛组阐述病毒感染调控的新机制
2017-10-28 BioArt BioArt
日前,Science杂志在线刊登了第二军医大学医学免疫学国家重点实验室、中国工程院院士曹雪涛研究团队题为“An Interferon-independent lncRNA promotes viral replication by modulating cellular metabolism”的研究论文,报道了非编码RNA lncRNA-ACOD1通过结合细胞内代谢酶GOT2调控胞内代谢促进病毒逃
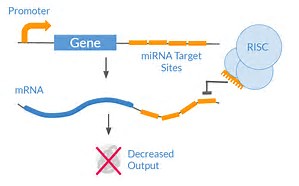
病毒感染调控一直以来是免疫学研究的热点。干扰素是机体抵抗病毒感染的关键性细胞因子,通过激活一系列干扰素诱导性基因的表达,从而激活机体的抗病毒能力。然而,干扰素以外的调控机制,尤其是病毒如何调控宿主细胞代谢的,目前知之甚少。
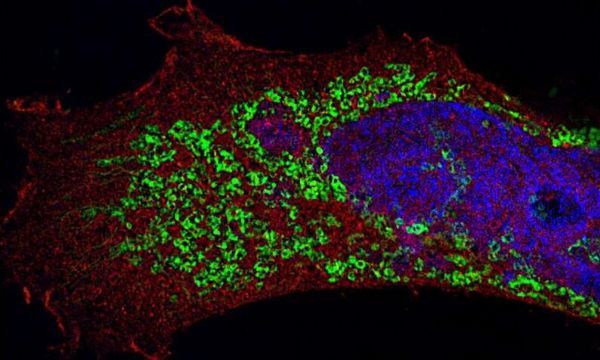
在国家自然科学基金委、中国医学科学院创新基金等资助下,医学免疫学国家重点实验室主任曹雪涛院士、王品副教授与浙江大学医学院免疫学研究所博士生徐俊芳等,从基因组中表达量很高但却功能未知的非编码RNA入手,筛选到其中一个lncRNA—lncRNA-ACOD1,在体内外均能显着的促进多种病毒的复制。深入研究发现lncRNA-ACOD1通过不依赖干扰素的一条新作用模式促进病毒感染,表达谱检测显示代谢通路受到lncRNA-ACOD1的明显调控。分子机制上,lncRNA-ACOD1在细胞浆中结合代谢中重要的氨基转移酶GOT2,在分子构象上靠近酶底物结合位点,有利于其催化反应。体外酶活性实验和体内LC-MS质谱代谢物检测证实lncRNA-ACOD1能够促进GOT2的代谢活性,且GOT2缺失则lncRNA-ACOD1促进病毒复制的功能丧失,补充GOT2或其催化底物能够逆转lncRNA-ACOD1缺失造成的病毒复制减弱。这证实lncRNA-ACOD1通过促进GOT3酶活性影响代谢,促进了病毒复制的作用模式。
该研究揭示了病毒感染通过lncRNA调控细胞代谢的新机制,解释了病毒调控代谢的分子机制,为临床上研发新的抗病毒药物提供了潜在的研究靶标。同时进一步完善了病毒感染调控网络,提出了干扰素之外的病毒感染调控新通路,将非编RNA、代谢调控和病毒感染三者联系在了一起,为免疫调控机制的研究提供了新的思路。
值得一提的是,该工作为曹雪涛课题组在LncRNA领域发表的第二篇Science论文,而且两篇论文的第一作者均为王品博士。王品博士现为海军军医大学(第二军医大学)免疫学研究所暨医学免疫学国家重点实验室副教授,国家优青。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#曹雪涛#
95
#SCIE#
77
学习了新知识
101
学习了新知识学习了新知识
99
学习了.谢谢分享.
78