第24届EHA大会:5F9联合利妥昔单抗治疗复发难治性非霍奇金淋巴瘤的Ib / II期临床试验
2019-06-18 Allan MedSci原创
Forty Seven是一家临床阶段的生物制药公司,专注于开发癌症免疫疗法,Forty Seven近日宣布其正在进行的Ib/II期临床试验的最新数据将在第24届欧洲血液学协会(EHA)大会上公布,以评估5F9与利妥昔单抗联合治疗复发难治非霍奇金淋巴瘤(包括弥漫性大B细胞淋巴瘤和惰性淋巴瘤)的有效性和安全性。
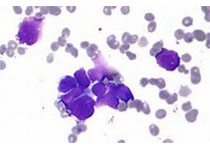
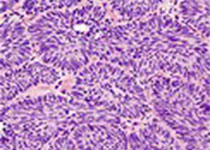
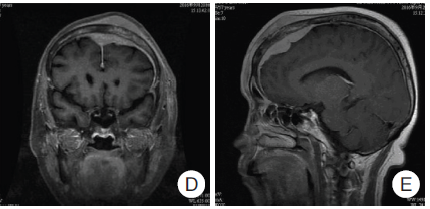
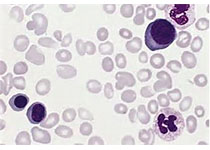
Forty Seven是一家临床阶段的生物制药公司,专注于开发癌症免疫疗法,Forty Seven近日宣布其正在进行的Ib/II期临床试验的最新数据将在第24届欧洲血液学协会(EHA)大会上公布,以评估5F9与利妥昔单抗联合治疗复发难治非霍奇金淋巴瘤(包括弥漫性大B细胞淋巴瘤和惰性淋巴瘤)的有效性和安全性。同样在EHA,Forty Seven将提供其正在进行的Ib期临床试验的数据,该试验评估了5F9作为单药或与阿扎胞苷联用以治疗骨髓增生异常综合征(MDS)和急性髓性白血病(AML)的有效性。
芝加哥大学医学博士、临床试验研究员Justin Kline说:“尽管初治NHL的治疗取得了进展,但对于晚期NHL患者的治疗选择非常有限。在治疗这些患者时,我们的目标是实现持久的反应并避免快速的疾病进展”。
原始出处:
http://www.firstwordpharma.com/node/1647714#axzz5rAF78auR
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#复发难治#
76
#I期临床试验#
84
#I期临床#
81
#II期临床试验#
69
#利妥昔#
69
#EHA#
67
#II期临床#
80
#难治性#
61