SCRT:脐带来源间充质干细胞治疗中国成人2型糖尿病的有效性和安全性
2022-05-20 从医路漫漫 MedSci原创
间充质干细胞(MSCs)是一种成体干细胞,通过分泌多种细胞因子和免疫抑制分子而具有强大的抗炎和免疫调节能力。
背景:2型糖尿病(T2DM)是一种异质性综合征,其特征在于由胰岛素敏感性降低和胰岛素分泌减少引起的血糖控制的进行性恶化,由于其高患病率和严重的发病率,它已经成为世界范围内对人类健康的严重威胁。饮食控制、体育锻炼和降糖药物已被证明可暂时改善高血糖症,但不能抑制T2DM的发病或降低其发病率。因此,需要开发更有效的方法来治疗T2DM。
间充质干细胞(MSCs)是一种成体干细胞,通过分泌多种细胞因子和免疫抑制分子而具有强大的抗炎和免疫调节能力。它们已成功应用于治疗不同类型的自身免疫性疾病,如中风、心肌梗死、类风湿性关节炎、系统性红斑狼疮和移植物抗宿主病。胰岛素敏感组织和胰岛的慢性炎症反应和免疫紊乱导致胰岛素抵抗、胰岛β细胞破坏和T2DM病的发生。因此,骨髓间充质干细胞移植可能是T2DM的一种治疗选择。以前的动物研究表明,MSCs治疗通过促进胰岛恢复和减轻胰岛素抵抗来改善高血糖症。此外,越来越多的临床试验报道了骨髓间充质干细胞移植治疗T2DM患者的疗效和安全性。MSCs可以来源于各种组织(例如骨髓、脂肪组织和脐带),并且MSCs的获取或使用被认为是无争议的。首先从骨髓中分离出间充质干细胞,骨髓被认为是治疗T2DM最容易获得的间充质干细胞来源。几项临床试验已经证实了骨髓间充质干细胞(BM-MSCs)在T2DM的治疗潜力。脐带来源的间充质干细胞(UC-MSCs)具有与骨髓间充质干细胞相似的免疫抑制特性,并因其低成本、无痛、高产、快速收集和无免疫原性的特点而具有T2DM的临床潜力。然而,很少有临床研究关注UC-MSCs治疗T2DM,也没有临床试验报道UC-MSCs对T2DM患者胰岛素抵抗的影响。因此,我们进行了一项单中心、随机、双盲、安慰剂对照的II期试验,以探讨T2DM患者静脉输注UC-MSCs的有效性和安全性。
方法:在这项单中心、双盲、随机、安慰剂对照的II期试验中,91名患者被随机分配接受UC-MSCs (n = 45)或安慰剂(n = 46)静脉输注三次,间隔4周,并从2015年10月至2018年12月随访48周。主要终点是48周时糖化血红蛋白(HbA1c)水平< 7.0%且每日胰岛素减少≥ 50%的患者百分比。其他终点是代谢控制、胰岛β细胞功能、胰岛素抵抗和安全性的变化。
结果:48周时,UC-MSCs组20%的患者和安慰剂组4.55%的患者达到主要终点(p < 0.05,95%可信区间(CI)2.25–28.66%)。UC-MSCs组的胰岛素减少百分比显著高于安慰剂组(27.78%对15.62%,p < 0.05)。UC-MSCs组HbA1c水平下降1.31%(9.02±1.27%至7.52±1.07%,p < 0.01),而安慰剂组仅下降0.63%(8.89±1.11%至8.19±1.02%,p˃0.05;两组之间p = 0.0081)。UC-MSCs组的葡萄糖输注率(GIR)显著增加(从3.12到4.76 mg/min/kg,p < 0.01),而安慰剂组没有观察到显著变化(从3.26到3.60 mg/min/kg,p˃0.05;两组间p < 0.01)。两组的胰岛β细胞功能都没有改善。没有发生与UC-MSCs移植相关的主要不良事件。
表1在9-48周的随访中,HbA1c水平< 7.0%且每日胰岛素减少≥ 50%的患者百分比
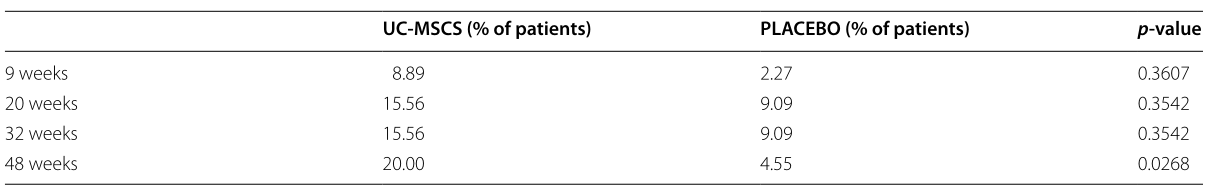

图1 UC-MSCs或安慰剂治疗后的胰岛素需求和HbA1c水平。*两组之间p < 0.05,**p < 0.01,***p < 0.001。
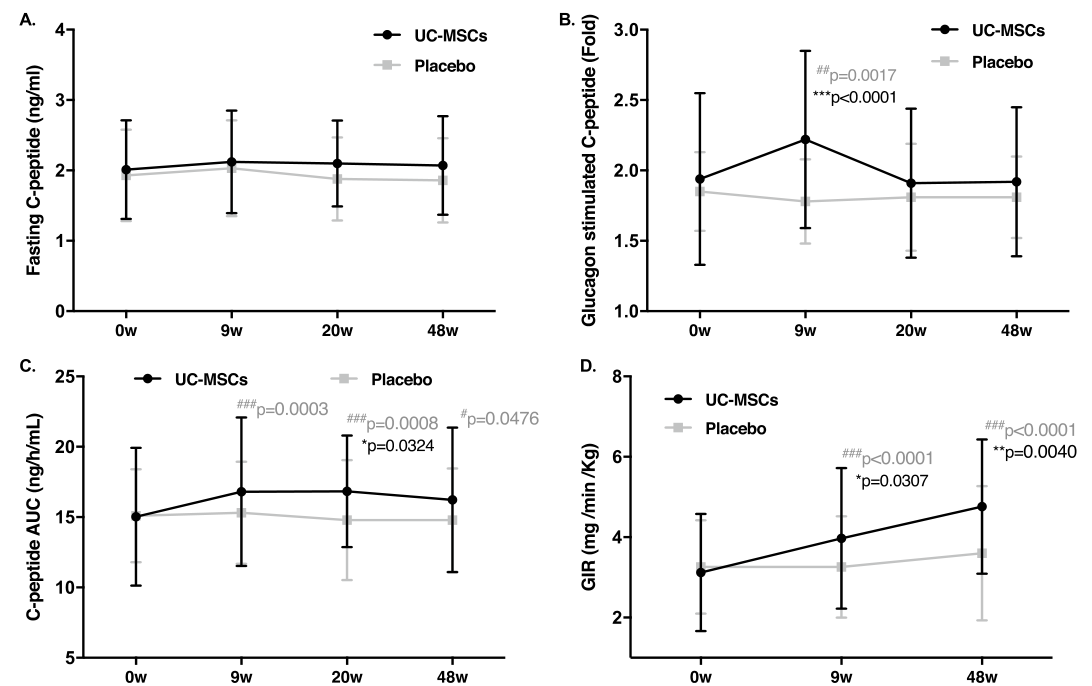
图2是UC-MSCs或安慰剂治疗后胰岛β细胞功能和胰岛素抵抗。*两组间p < 0.05,**p < 0.01,* * * p < 0.001# p < 0.05# # p < 0.01# # #与基线值相比p < 0.001。GIR,葡萄糖输注率
结论:UC-MSCs移植可能成为中国成人T2DM的一种潜在治疗方法。
原文出处:Zang L, Li Y, Hao H, Liu J,et al.Efficacy and safety of umbilical cord-derived mesenchymal stem cells in Chinese adults with type 2 diabetes: a single-center, double-blinded, randomized, placebo-controlled phase II trial.Stem Cell Res Ther 2022 May 03;13(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#间充质干细#
63
#成人2型糖尿病#
63
#CRT#
60
#脐带#
57
#SCR#
63