NAT COMMUN:表观调节剂Mll1驱动肠道肿瘤发生和干性
2020-12-24 haibei MedSci原创
研究人员发现,组蛋白甲基转移酶Mll1是Wnt驱动的肠癌的调节器。Mll1在Lgr5+干细胞和人结肠癌中高表达,这些细胞的核内β-catenin也有所增加。高水平的MLL1与结肠癌患者的生存率差有关。
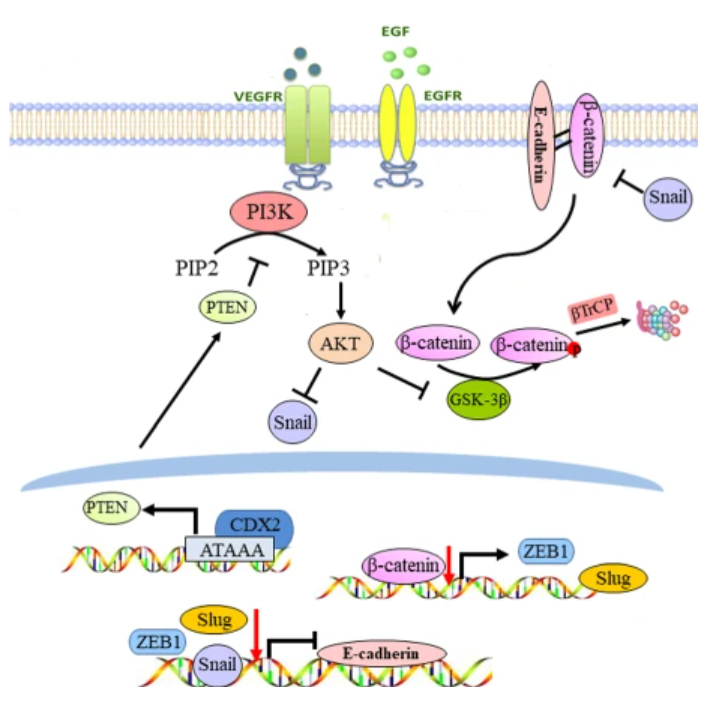
Wnt/β-catenin信号可以控制成体干细胞的自我更新,并促进肿瘤发生。已有的研究显示,激活的Wnt/β-catenin信号与结肠癌以及许多其他人类癌症有关。由APC,Gsk3β和Axin1/2组成的破坏复合物的失活可以稳定β-catenin,否则β-catenin会被磷酸化和泛素化的蛋白酶体降解。稳定的β-catenin会转位到细胞核,并结合到Tcf / Lef1转录因子上,诱导靶基因的表达,如Axin2。Wnt信号元件的突变通过促进β-catenin的异常稳定性和超活性来启动肠道肿瘤的发生。

最近,研究人员发现,组蛋白甲基转移酶Mll1是Wnt驱动的肠癌的调节器。Mll1在Lgr5+干细胞和人结肠癌中高表达,这些细胞的核内β-catenin也有所增加。高水平的MLL1与结肠癌患者的生存率差有关。
在Lgr5+肠干细胞中,Mll1基因的敲除可以防止的Wnt/β-catenin驱动的腺瘤形成。Mll1的敲除也可以降低人结肠癌的自我更新,并阻止异种移植的肿瘤生长。
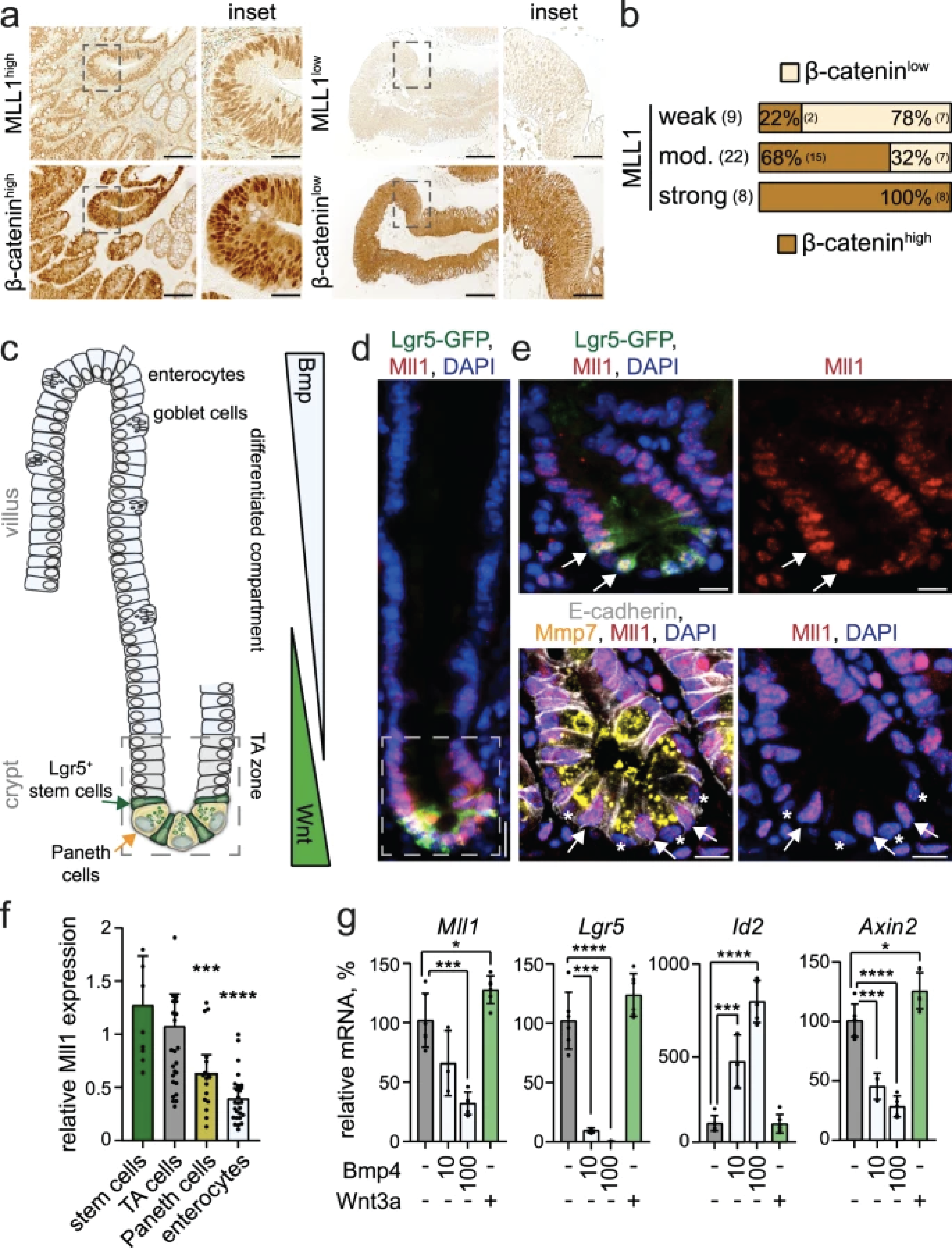
Mll1控制干细胞基因的表达,包括Wnt/β-catenin靶基因Lgr5。Mll1丢失后,干细胞启动子处的组蛋白甲基化从激活性的H3K4三甲基化转换为抑制性的H3K27三甲基化,表明Mll1通过多聚抑制复合物2(PRC2)介导的H3K27三甲基化拮抗基因沉默,从而维持干细胞基因的表达。
对Wnt突变的肠道肿瘤启动细胞的转录组剖析显示,Mll1调控Gata4/6转录因子,已知Gata4/6转录因子可维持癌症细胞干性并控制小叶细胞分化。
因此,该研究结果表明,Mll1是Wnt/β-catenin诱导的肠道肿瘤发生和干性维持的重要表观遗传调节因子。
原始出处:
Johanna Grinat et al. The epigenetic regulator Mll1 is required for Wnt-driven intestinal tumorigenesis and cancer stemness. NATURE COMMUNICATIONS (2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#COMMUN#
54
#肠道肿瘤#
74
#Nat#
51
#MLL1#
57
表观调节剂Mll1驱动肠道肿瘤发生和干性
124