BMJ:非创伤性ARDS出现巨大纵隔气肿——病例报道
2016-01-26 MedSci MedSci原创
男性患者,曾患有急性呼吸窘迫综合征现已恢复,接受压力通气支持(压力20 cm H2O,PEEP = 8 cm H2O)。现在患者右侧锁骨上窝出现皮下气肿。
男性患者,曾患有急性呼吸窘迫综合征现已恢复,接受压力通气支持(压力20 cm H2O,PEEP = 8 cm H2O)。现在患者右侧锁骨上窝出现皮下气肿。
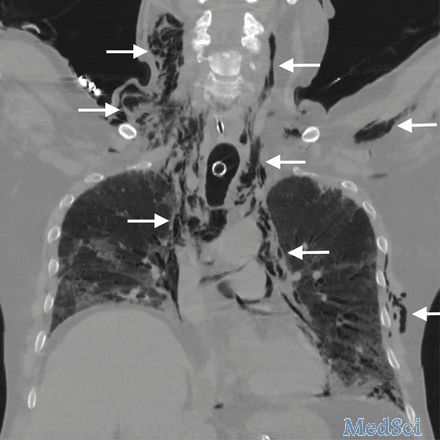
胸部CT显示一个巨大的纵隔气肿,而并无气胸的表现(如下图所示),与Macklin效应的表现相符,Macklin效应是指钝性肺泡破裂,空气进入支气管血管鞘,还可进入纵膈(如箭头所示)。尽管Macklin效应通常发生于创伤后,但是有时也可发生于低PEEP值下的机械通气患者。

由于患者并没有出现气胸及纵膈偏移的现象,故采取保守治疗,但是有些病例需要进行胸腔引流和气管切开。
原始出处:
Davide Durí, Amato De Monte, Francesco Toso. Massive pneumomediastinum after non-traumatic ARDS. BMJ 2016; 352 doi: http://dx.doi.org/10.1136/bmj.i360 (Published 25 January 2016)Cite this as: BMJ 2016;352:i360.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#BMJ#
61
#创伤性#
71
#RDS#
63
#创伤#
74