Sci Rep:一项关于膀胱填充预防多次剖宫产造成的粘连性疾病和膀胱损伤的随机对照试验
2020-09-30 AlexYang MedSci原创
剖宫产术有膀胱损伤的风险,因为粘连的形成遮蔽了盆腔平面。在膀胱被逆填充(cystoinflation)时显像使其容易辨认,因为其紧致的圆形轮廓上升到了腹腔。
剖宫产术有膀胱损伤的风险,因为粘连的形成遮蔽了盆腔平面。在膀胱被逆填充(cystoinflation)时显像使其容易辨认,因为其紧致的圆形轮廓上升到了腹腔。
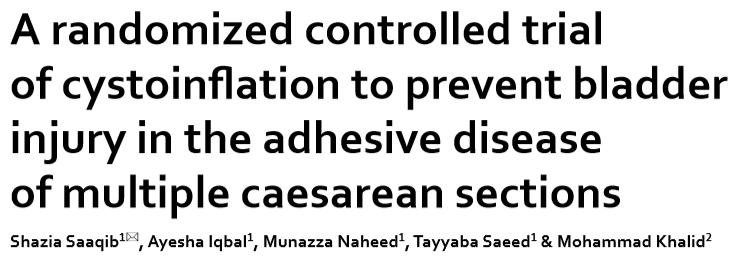
在近期发表在scientific reports期刊的一项研究中,来自巴基斯坦爱德华国王医学院的研究者们进行了一项前瞻性随机对照试验,探讨了通过膀胱逆填充改善膀胱边缘识别能否降低膀胱损伤率和失血,而不引起泌尿系统并发症。这项研究纳入了214名既往手术分娩的健康女性,她们曾接受择期剖腹产,并发现盆腔粘连严重。受试者被随机分为膀胱逆填充组和对照组。膀胱逆填充组通过使用300cc生理盐水逆填膀胱来进行粘连松解术,对照组不进行逆填。膀胱逆填充组膀胱损伤率明显低于对照组(2.8% vs 20.6%, P < .0001),出血量较小(585.33 cc vs 797.10 cc, P < .0001)。两组的平均手术时间相似。对照组尿路感染和排尿问题发生率高于膀胱膨胀组(分别为16.8% vs 1.9%,P = .001和0.47 ± 1.63% vs 0.77 ± .633%,P = .021)其中1例患者有瘘管,而膀胱逆填充组则没有。
主要结果和次要结果
本研究表明,膀胱逆填充可显著降低膀胱损伤率和出血量。这项技术也可能在外科、泌尿外科和妇科领域被证明发挥作用。
原始出处:
Saaqib, S., Iqbal, A., Naheed, M. et al. A randomized controlled trial of cystoinflation to prevent bladder injury in the adhesive disease of multiple caesarean sections. Sci Rep 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#对照试验#
78
#对照#
69
#随机对照试验#
73
#损伤#
73
RCT
122
学习
140
高质量研究,读起来真爽,谢谢梅斯
86