Blood:原发性嗜血性淋巴细胞增生症的无症状患儿的治疗瓶颈
2018-08-15 MedSci MedSci原创
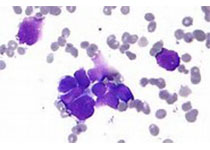
原发性嗜血性淋巴细胞增生症(HLH)的致病基因致病性等位基因突变的无症状携带者易患致命性HLH,需采用造血干细胞移植(HSCT)进行治疗。目前,尚无针对无症状患者的管理指南。Giovanna Lucchini等人对双指数病例(ICs)的预后进行分析,发现随后确诊的无症状家庭成员(ACs)也携带相同的遗传缺陷。研究人员从全球的22个HSCT中心收集相关数据,共筛选到32对(64位)患者可用于评估。I
Giovanna Lucchini等人对双指数病例(ICs)的预后进行分析,发现随后确诊的无症状家庭成员(ACs)也携带相同的遗传缺陷。研究人员从全球的22个HSCT中心收集相关数据,共筛选到32对(64位)患者可用于评估。ICs中HLH发病的中位年龄为16个月。32对ICs中有7对在一线治疗过程中死亡,仅两对活至化疗结束。23对患者进行HSCT治疗,其中16对存活。
确诊后中位随访36个月时,18对ICs仍存活。确诊时ACs的中位年龄为5个月。10对ACs在观察期间罹患HLH,均行HSCT治疗:其中6对存活,获得完全缓解(CR);另外22对患者保持无症状,其中6对未采取治疗,随访39个月时仍处于完全缓解,另16对患者直接采用HSCT治疗,15对患者完全缓解存活。未发病的ACs的8年总体存活率明显高于ICs(95% vs 45%,p=0.02),在发病前就采取HSCT的ACs的总体存活率明显高于HLH发病后进行HSCT治疗的ACs(93% vs 64%,p=0.03)。
现已证实,在HLH发病前,ACs即采取HSCT治疗可安全有效提高其长期预后,值得考虑。
原始出处:
Giovanna Lucchini,et al. Treatment dilemmas in asymptomatic children with primary haemophagocytic lymphohistiocytosis. Blood 2018 :blood-2018-01-827485; doi: https://doi.org/10.1182/blood-2018-01-827485
本文系梅斯医学(MedSci)原创编译,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#原发性#
59
#淋巴细胞#
56
#无症状#
60
原发性嗜血性淋巴细胞增生症的治疗。
99
不错的文章值得拥有哦
76
了解一下,谢谢分享!
121
学习了
100
学习了,涨知识了!
101