Arthritis & Rheum:尹芝南等发现治疗小鼠类风湿关节炎的小分子化合物
2012-05-19 南开大学生科院 南开大学生科院
近日,国际重要学术期刊《Arthritis & Rheumatism》(关节炎研究领域排名第一,影响因子8.435)在线刊登了南开大学生科院尹芝南教授课题组的最新研究成果“Therapeutic effects of a novel Tylophorine analog NK-007 on collagen-induced arthritis through suppressing TNF
近日,国际重要学术期刊《Arthritis & Rheumatism》(关节炎研究领域排名第一,影响因子8.435)在线刊登了南开大学生科院尹芝南教授课题组的最新研究成果“Therapeutic effects of a novel Tylophorine analog NK-007 on collagen-induced arthritis through suppressing TNF-α production and Th17 differentiation†,”,该成果发现了能够治疗小鼠类风湿关节炎的新的小分子化合物。
类风湿关节炎为一种临床上最常见的疑难顽症,进程性的关节损伤最终可导致关节的畸形、肢体残疾甚至使患者失去活动能力。随着免疫学的发展,对于细胞因子在关节炎症和损伤中起着重要作用的认识使得靶向特定细胞因子的新型治疗药物应用于临床,并且对于患有关节炎病的治愈具有重要的影响。
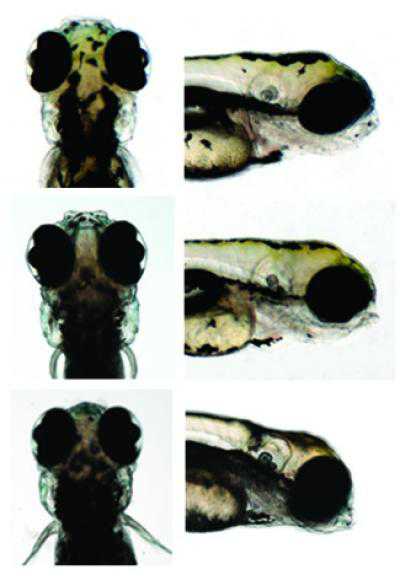
尹芝南教授课题组博士生温倜在前期工作的基础上,通过对化学学院汪清民教授提供的多种DCB-3503衍生物进行筛选,发现一种新的小分子化合物NK (nankai)-007通过抑制p38的磷酸化,降低p38下游MK2水平,并促进锌指蛋白36的表达,从而在转录后水平拮抗多种免疫细胞产生TNF-a;并对初始CD4+T细胞分化为Th17有抑制作用。应用NK-007可以预防及治疗小鼠胶原诱导的关节炎发病。该项研究发现了治疗小鼠类风湿关节炎的一个新药物,有助于研发用于治疗人类类风湿关节炎的新型生物制剂。该项工作得到国际合作交流项目、973国家重点基础研究发展计划和南开大学科技处的资助。

doi:10.1002/art.34528
PMC:
PMID:
Therapeutic effects of a novel Tylophorine analog NK-007 on collagen-induced arthritis through suppressing TNF-α production and Th17 differentiation†
Ti Wen Ph.D. candidate1, Yangguang Li Ph.D. candidate1, Meng Wu Ph.D. candidate2, Xiaolin Sun Ph.D.3, Xiucong Bao B.S.1, Yuquan Lin Ph.D. candidate1, Jianlei Hao Ph.D. candidate1, Lin Han M.S. candidate1, Guangchao Cao Ph.D. candidate1, Ziwen Wang Ph.D.2, Yuxiu Liu Ph.D.2, Zhenzhou Wu Ph.D.1, Zhangyong Hong Ph.D.1, Puyue Wang Ph.D.1, Liqing Zhao Ph.D.1, Zhanguo Li M.D., Ph.D.3, Qingmin Wang Ph.D.2,‡,*, Zhinan Yin M.D., Ph.D.1,*
Objective. To analyze the effects of a novel compound NK-007 on the prevention and treatment of collagen-induced arthritis (CIA) and the underlying mechanisms. Methods. The effect of NK-007 on lipopolysaccharides (LPS)-triggered tumor necrosis factor-α (TNF-α) production by murine splenocytes and macrophage cell line (Raw 264.7) was determined by ELISA, intracellular cytokine staining as well as Western Blot. LPS-boosted CIA model was adopted and NK-007 or vehicle was administered at different time points post immunization and the mice were monitored for the clinical severity, the joint tissues were used for histological examination, cytokine detection and immunohistochemical staining. Finally, stability of TNF-α and Th17 differentiation were studied using qPCR and flow cytometry. Results. NK-007 significantly suppressed LPS-induced TNF-α production in vitro. Administration of NK-007 completely blocked CIA development and progression. Furthermore, treatment with NK-007 at the onset of arthritis significantly inhibited the progress of joint inflammation. Administration of NK-007 also suppressed production of TNF-α, IL-6 and IL-17A in joint, and reduced IL-17 positive cells in CD4+ and γδ T cells in draining lymph nodes. We further demonstrated that NK-007 acted on the stability of TNF-α mRNA, and reduced Th17 differentiation. In addition, it significantly inhibited IL-6 and IL-17A level in human co-culture assay. Conclusion. For its effects on the development, progression and therapeutic effect on CIA, NK-007 has a great potential to be a therapeutic agent for human RA. © 2012 American College of Rheumatology.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#小分子#
71
#化合物#
66
#Arthritis#
61
#关节炎#
57
#类风湿#
49
#ART#
53
#风湿关节炎#
61