Opdivo/Cabometyx组合疗法用于一线治疗晚期肾癌的III期临床实验成功
2020-04-22 MedSci原创 MedSci原创
"如果获得批准,这种组合可能成为转移性肾细胞癌患者重要的一线治疗新选择。"
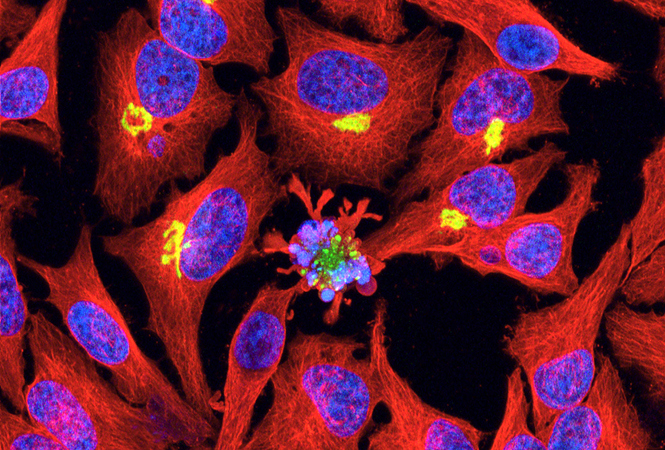
Bristol Myers Squibb和Exelixis公司宣布,PD-1单抗Opdivo(nivolumab)和酪氨酸激酶抑制剂Cabometyx(cabozantinib)联合治疗的III期临床试验,已达到其延长肾癌患者无进展生存期的主要目标。
CheckMate-9ER III期临床试验正在评估与舒尼替尼相比,cabozantinib和nivolumab组合在先前未接受治疗的晚期或转移性肾细胞癌(RCC)患者中的疗效和安全性。
cabozantinib和nivolumab组合未发现新的安全问题。
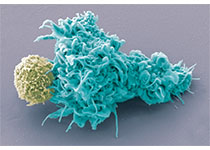
Exelixis产品开发和医疗事务总裁兼首席医疗官Gisela Schwab说:"鉴于越来越多的数据表明cabozantinib可以调控肿瘤环境,从而增强患者对免疫检查点抑制剂的应答,我们一直热切期待cabozantinib和nivolumab联合用于先前未经治疗的肾细胞癌患者中的实验结果。"
达纳-法伯癌症研究所的Toni Choueiri博士表示:"关键的CheckMate-9ER试验结果清楚地表明,cabozantinib和nivolumab的组合显著改善了先前未接受过治疗的肾癌患者的无进展生存期和总体生存期的关键疗效指标。"
"如果获得批准,这种组合可能成为转移性肾细胞癌患者重要的一线治疗新选择。"
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#临床实验#
79
#I期临床#
72
#III#
61
#MET#
91
#组合疗法#
88
#Opdivo#
71
#晚期肾癌#
117
#II期临床#
65
#III期#
99
#ABO#
90