Translational Psychiatry:岛叶形态学改变与精神障碍临床表型相关
2021-06-06 MedSci原创 MedSci原创
该研究发现较小的脑岛体积在精神病中遵循前后梯度,并为精神病谱障碍提供广泛的风险。脑皮质褶皱减少是精神分裂症特有的,可能反映出产前发育的改变导致认知障碍。
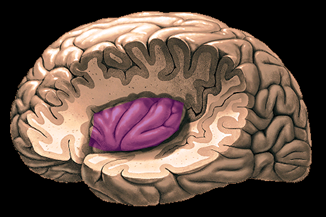
脑岛是位于大脑侧裂深处的异质大脑结构,涉及大量的人类行为和精神体验。脑岛常被认为是大脑的第五叶,是第一个发育和分化的皮质区域,从胎儿出生六周开始。岛叶是一个异质性皮质区域,由三个细胞结构不同的亚区域(颗粒状、非颗粒状和颗粒状)组成,它们横贯前后轴,不同程度地参与情感、认知和体感处理。由于脑岛在各种认知、情感和调节功能中的不同作用,它与精神疾病的关系越来越密切,特别是在精神疾病中的作用。脑岛异常在精神疾病中普遍存在,包括结构改变、异常静息状态功能连接和基于任务的激活改变。在精神病谱系障碍中,岛叶体积较小的报道是一致的,并被推测部分原因是神经发育异常。
为了更好地了解精神疾病中岛叶异常的区域和诊断特异性,它们的发展病因和临床相关性,Julia M. Sheffield等对一大批成年精神障碍患者(精神分裂症谱系,精神分裂症谱系)的岛叶体积和形态进行了特征分析。提出了以下目标:(1)描述精神病谱系中岛叶亚区域的体积和表面形态,(2)确定这些改变的诊断特异性,以及(3)检查对临床表型的贡献。该研究结果发表在Translational Psychiatry杂志。
纳入对象为成人精神障碍患者(精神分裂症谱系,精神双相障碍)和社区确定的青年精神谱系队列(8-21岁)。使用计算解剖学工具箱(CAT12)从T1加权的脑结构图像中定量脑岛体积和形态(皮质厚度、皮层折叠褶皱、沟回深度)。
在费城神经发育队列(PNC)中,健康成年人(n = 196)、精神障碍患者(n = 303)和1368名个体(381名典型发展(TD)、381名青年精神病谱系(PS)、606名青年其他精神病理(OP))接受了调查。
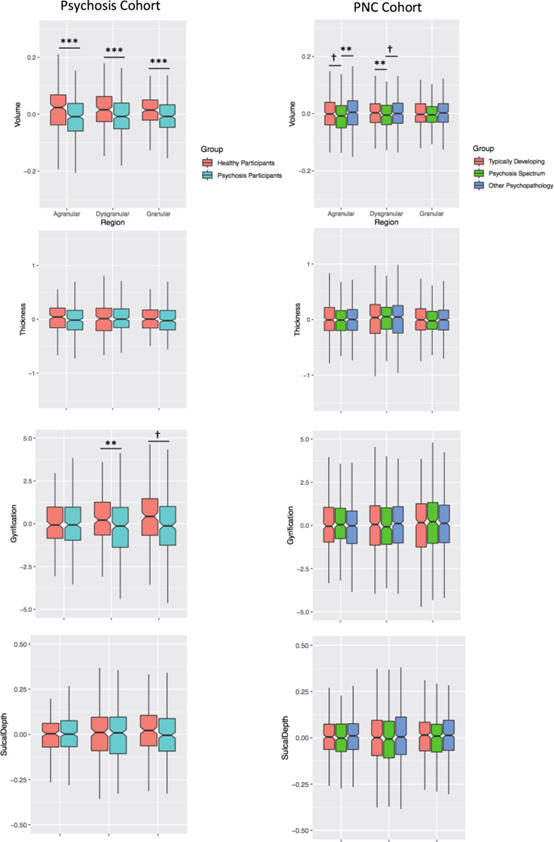
基于感兴趣区域分析的脑岛体积和表面特征。精神病患者和精神病谱系青年表现出岛叶亚区体积减少,遵循前后梯度。根据HCP-MMPI图谱66的分块,从颗粒子区域提取基于表面的形态测量值。在精神病患者队列中,只观察到非颗粒状旋转的显著改变。给出了边际均值。协变量包括年龄、性别、总颅内容积(TIV)、研究(用于精神病患者队列)和地形缺陷(用于基于表面的测量)。***p < 0.001, **p < 0.017, †p < 0.05 但没有通过多次比较校正。
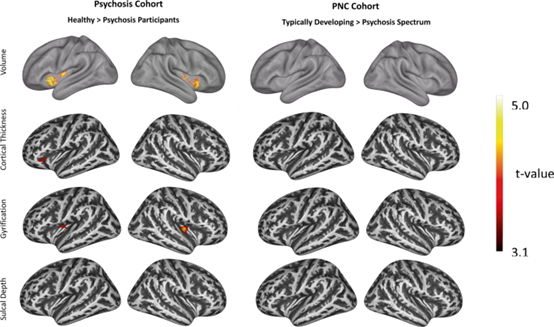
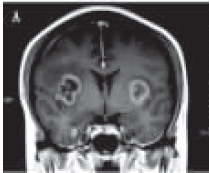
基于体素和顶点分析的脑岛体积和表面特征。为了补充感兴趣区分析,使用显式岛叶掩码对每个队列的岛叶结构进行了体素(体积)和顶点(表面)分析。在精神病(健康对照精神病)和PNC(典型发展中的精神病青年)队列中显示了组间的差异。反映和扩展感兴趣区分析,精神障碍的参与者体积和褶皱减少,以及皮质厚度减少。NC组间差异无统计学意义。在体素层面校正的pFWE = 0.05;未校正的pFWE = 0.001,控制了年龄、性别、总颅内容积(TIV)、研究(用于精神病队列)和地形缺陷(用于基于表面的测量)。在精神障碍和PNC队列中,不规则体积与认知能力的相关性。体积以对照组、年龄、性别和总颅内体积(TIV)的边际平均值表示。
在两组中,较低的颗粒状岛叶体积与较差的整体认知能力相关,其效应大小高度相似。成年精神障碍患者和青少年精神谱系障碍患者的脑岛体积显著减小,呈前后梯度分布。形态异常仅限于精神障碍患者的皮层折叠褶皱减少,这是精神分裂症特有的,与认知能力相关。脑岛的体积和厚度与认知、阳性和阴性精神病症状相关。
该研究分析了成人精神障碍(精神分裂症谱和精神双相障碍)和青年精神障碍谱症状的脑岛亚区域体积、形态和临床相关性。在精神障碍患者和精神病谱系青少年中,脑岛体积较小,并且在两组中都与认知障碍相关。对岛叶亚区域的调查显示,较小的岛叶体积在精神病谱系中具有前后梯度,较小的体积在岛叶前部更为明显。基于表面形态测量学的平行分析发现,精神障碍患者的脑回褶皱较低,有少量证据表明皮质厚度或沟深减少。体积和褶皱减小只在精神分裂症中观察到,而不是精神双相障碍。非颗粒状亚区域褶皱减少,与认知缺陷相关。最后,在精神障碍中,阳性和阴性症状与多个颗粒亚区域的体积和厚度小相关,但与青年精神病谱无关。
这些发现表明,脑岛体积减少作为一种神经发育脆弱性,提供了广泛的精神病谱系障碍风险,并与临床表型,特别是认知障碍相关。另一方面,脑岛形态测定法对精神分裂症患者的脑回褶皱减少更为特异,这可能表明该人群存在早期神经发育异常。总之,在精神障碍和精神病谱系青少年中,脑岛体积减少,并与认知能力相关,这表明脑岛体积不足具有广泛的精神病风险。脑岛褶皱减少也见于精神障碍,但在精神分裂症中最为明显,并导致认知障碍。阴性和阳性症状也与岛叶亚区域结构有关,提示岛叶病理生理异常与临床表型有关。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Transl#
41
#Translation#
34
#translational#
46
#TRA#
50
#Psychiatry#
44
#临床表型#
46
#表型#
39
学习
57