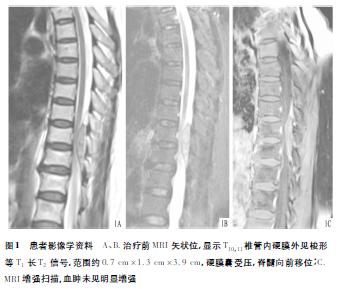
自发性椎管内硬膜外血肿1例
2018-12-03 陈士军 韩业福 付艳超 临床骨科杂志
患者,女,63岁,因突发双下肢麻木伴乏力14h余入院。主诉:在家弯腰洗衣服时突感胸腰背部疼痛,双下肢麻木、无力,不能站立及行走,无昏迷、恶心及低热、盗汗等伴随症状。急至当地医院行胸椎X线及CT检查,未见明显异常,予以局部康复理疗后未见好转,且症状逐渐加重。我院门诊以“不全瘫”收住我科。患病以来,患者精神尚可,大、小便未解。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#硬膜外血肿#
76
#硬膜外#
54
#椎管#
64
#椎管内#
67
#血肿#
67
#自发性#
53