Blood:MYC和BCL2拷贝数变异对DLBCL肿瘤形态的影响及MYC-IHC假阴性的机制
2020-11-12 MedSci原创 MedSci原创
当世界卫生组织(WHO)将具有MYC、BCL2和/或BCL6重排的高度恶性B细胞淋巴瘤(HGBL-DH/TH)定义为临床类别时,重排是唯一纳入的结构变异(SV)。拷贝数变异(CNV)是另一种SV,常与
当世界卫生组织(WHO)将具有MYC、BCL2和/或BCL6重排的高度恶性B细胞淋巴瘤(HGBL-DH/TH)定义为临床类别时,重排是唯一纳入的结构变异(SV)。拷贝数变异(CNV)是另一种SV,常与基因异常表达有关。已经提出的一种“非典型双重打击”实体,涵盖除了共发生易位以外同时存在MYC和BCL2结构变异的肿瘤。虽然携带MYC和BCL2重排的肿瘤之间共有的基因表达特征(DHITsig)证实了这两种肿瘤具有共同的生物学基础,但MYC和BCL2 CNV的生物学意义还需要进一步阐明。
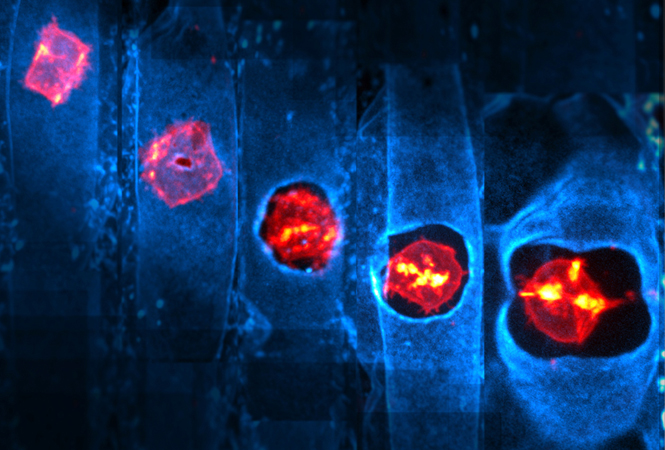
研究人员通过荧光原位杂交(FISH)对802例具有弥漫性大B细胞淋巴瘤(DLBCL)形态的新发肿瘤进行了MYC和BCL2 CNV的综合分析。
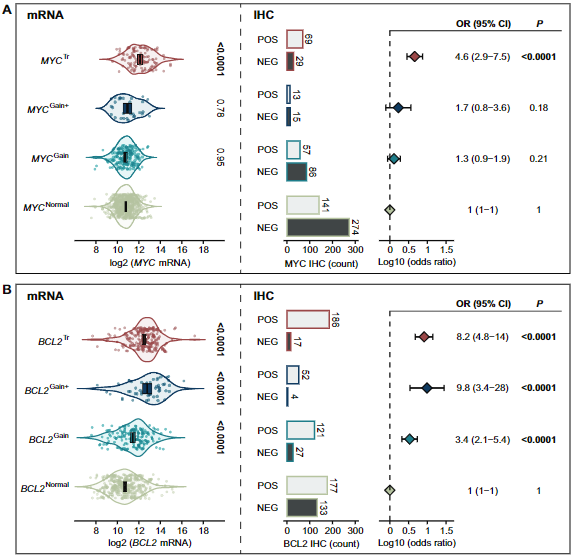
BCL2 CNV与表达增加相关,而MYC CNV则与表达增加无关。此外,在非典型双重打击的背景下,MYC和BCL2 CNV没有提供与HGBL-DH/TH-BCL2相似的基因表达谱。最后,虽然MYC IHC已被建议作为FISH检测的筛查工具,但研究人员观察到了MYC重排与IHC阳性解偶联的两种机制:1)MYC mRNA低表达;2)MYC基因第11位氨基酸残基(MYC-N11S)由单核苷酸多态性引起天冬酰胺-丝氨酸替代的免疫组织化学(IHC)染色呈假阴性。
综上所述,本研究结果支持目前从HGBL-DH/TH中排除MYC和BCL2 CNV的说法,并强调了基于分子的分类系统能够识别FISH和IHC未能完全捕获的具有共同生物学特征的肿瘤。
原始出处:
Collinge Brett J,Ben-Neriah Susana,Chong Lauren C et al. Impact of MYC and BCL2 structural variants in tumors of DLBCL morphology and mechanisms of false-negative MYC IHC. Blood, 2020. DOI:10.1182/blood.2020007193
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#拷贝数#
87
#拷贝数变异#
105
#LBCL#
59
#MYC#
83
#变异#
69
#DLBCL#
84
#BCL2#
72
评论怎么不成功呢
115
机制研究离临床仍然有距离,不过与临床结合思考,仍然有帮助的,不能仅仅是纯临床思维,转化思维同样重要
110
喜欢梅斯医学,分享知识
106