BMJ:至今仍盛行的一种历史性疾病-案例报道
2017-03-24 xing.T MedSci原创
维生素C水平进行了检查,由于高度的临床怀疑开始口服抗坏血酸(100mg,三次日常)。接下来证实维生素C水平<5μmol/L(正常范围为15-90 μmol/L)。病人由营养师进行了评估,出院后伴随社区营养师随访计划。四周后患者疲劳和皮肤改变消失。6周后复查全血液计数,血红蛋白水平正常。
患者为一名79岁男性,被他的全科医生转诊至医疗评估组。之前四周该患经历了双小腿进展性变色。其全科医生怀疑为蜂窝组织炎给予两个疗程的抗生素治疗但无临床改善。该患者整体较好,没有发热史。他否认有腿部外伤,无皮肤病史,也没有服用常规药物。男人独自生活且完全独立,其饮食中缺乏水果蔬菜。

检查发现脉搏、血压和氧饱和度正常,没有发热。胸部和腹部检查无异常。小腿到处都是瘀伤(瘀斑),并有“树皮样”水肿(如图1所示)。检查更近端腿部毛囊周围的出血和“螺旋”状毛发(图2,图3)。右腿比左大,但小腿软而无压痛。

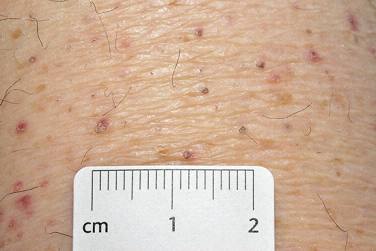
图3 右侧膝关节以上放大的皮肤改变
检查凝血功能、肾功能及肾功能检查均正常。腿部多普勒超声显示没有深静脉血栓形成的证据。尿液分析是正常的。全血液计数显示血红蛋白为117g/L是正常红细胞性贫血(130-180 g/L),但血小板计数正常。B12、叶酸和铁蛋白水平正常。
问题
1、最可能的诊断是什么?
维生素C缺乏症(坏血病)
2、进一步需要哪些检查?
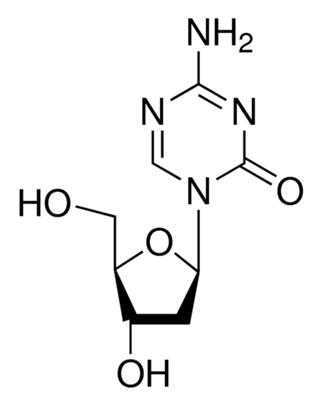
坏血病是临床诊断,但血清抗坏血酸(维生素C)水平<11μmol/L(正常范围为15-90μmol/L)确认缺乏。
3、这种疾病如何治疗?
口服抗坏血酸将提供症状缓解,额外的抗坏血病饮食将被建议。
患者预后
维生素C水平进行了检查,由于高度的临床怀疑开始口服抗坏血酸(100mg,三次日常)。接下来证实维生素C水平<5μmol/L(正常范围为15-90 μmol/L)。病人由营养师进行了评估,出院后伴随社区营养师随访计划。四周后患者疲劳和皮肤改变消失。6周后复查全血液计数,血红蛋白水平正常。
原始出处:
Lorne V Mitchell. et al. A historic disease still prevalent today. BMJ2017;356:j1013 doi: 10.1136/bmj.j1013
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#BMJ#
76
学习了谢谢分享
112
谢谢分享学习了
109
好资源
124
学习了谢谢分享
124
好资源
166
现在这种病非常少见
79
好资源
64
好资源
69
学习了谢谢分享
82