AJG:炎症性肠病患者中静脉血栓栓塞性疾病的发病率明显增高
2021-07-16 MedSci原创 MedSci原创
已知,炎症性肠病 (IBD) 患者的静脉血栓栓塞 (VTE) 疾病风险会比正常人高 3 倍以上,年轻的 IBD 患者的相对风险最大
已知,炎症性肠病 (IBD) 患者的静脉血栓栓塞 (VTE) 疾病风险会比正常人高 3 倍以上,年轻的 IBD 患者的相对风险最大,但 60 岁以上 IBD 患者的总体绝对风险最高。因此,如果住院 IBD 患者的血栓得到广泛预防,并且更有效的药物和更早的干预策略加强了活动性疾病的治疗,IBD 患者中 VTE 的发生率应该能显着下降。因此,本项研究旨在确定过去 30 年 IBD 中 VTE 的发生率是否有所降低。

研究人员使用基于人群的IBD 流行病学数据库(1984-2018)来确定 IBD 中 VTE 的发病率以及与匹配对照的发病率比。对于伴有和不伴有 VTE 的 IBD 患者,通过多变量逻辑回归评估了与 VTE 风险增加相关的变量。
研究结果显示IBD 队列中 VTE 的发生率为 7.6%,显着高于对照组(3.3%,P < 0.0001)。IBD 中 VTE 的总体年龄标准化发病率为 433/100,000,对照组为 184/100,000。克罗恩病 (8.4%) 的 VTE 发生率高于溃疡性结肠炎 (6.9%, P = 0.0028)。IBD 与对照组的发病率比为 2.36(95% 置信区间 2.16-2.58)。与溃疡性结肠炎相比,男性和女性以及克罗恩病的风险增加相似。1985年至2018年IBD患者发病率下降非常缓慢,年百分比变化为-0.7%(P= 0.0003)。使用肿瘤坏死因子抗体不到 3 年直至 VTE,以及类固醇和肿瘤坏死因子抗体的联合使用增加了 VTE 的风险。
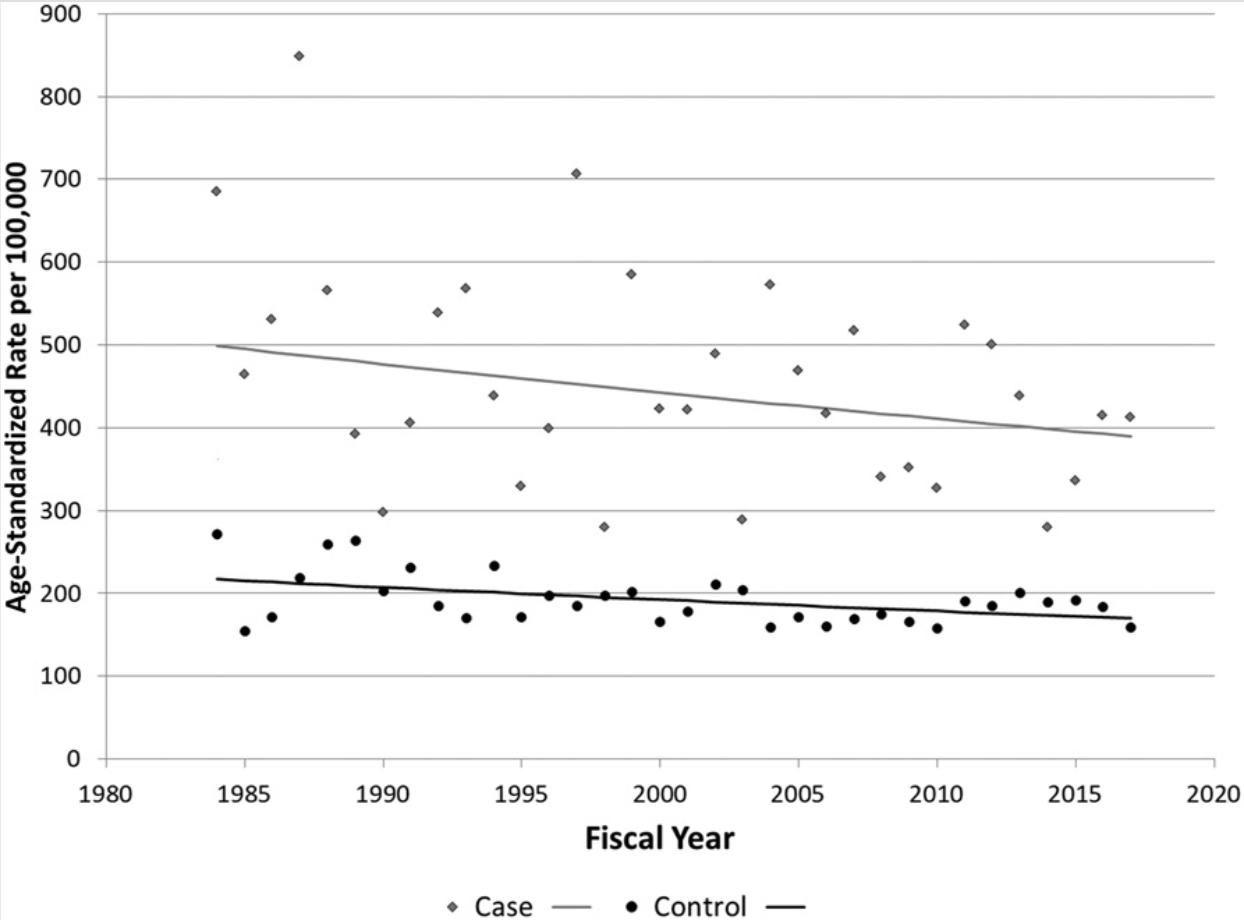
图:炎症性肠病患者中静脉血栓栓塞性疾病的发病率
本项研究证实尽管在过去 30 年中 IBD 管理取得了进步,但与对照组相比,VTE 的发生率只是缓慢下降并且仍然显着增加。
原始出处:
Bernstein, Charles N. et al, Persistently High Rate of Venous Thromboembolic Disease in Inflammatory Bowel Disease: A Population-Based Study. The American Journal of Gastroenterology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#静脉血#
88
#静脉血栓栓塞性#
92
#静脉血栓栓塞性疾病#
87
#静脉#
75
#AJG#
65
学习的
157
#发病率#
72
#炎症性#
60
#增高#
63
#增高#
72