European Radiology:CT放射组学列线图对腭扁桃体鳞状细胞癌和非霍奇金淋巴瘤的鉴别诊断
2021-11-03 shaosai MedSci原创
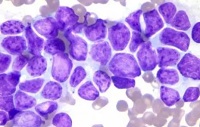
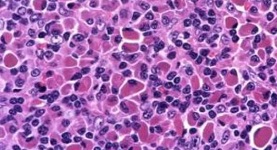
鳞状细胞癌(SCC)是头颈部最常见的恶性肿瘤,而非霍奇金淋巴瘤(NHL)是第二常见的肿瘤。腭扁桃体是头颈部SCC和NHL最常见的解剖学部位。这

鳞状细胞癌(SCC)是头颈部最常见的恶性肿瘤,而非霍奇金淋巴瘤(NHL)是第二常见的肿瘤。腭扁桃体是头颈部SCC和NHL最常见的解剖学部位。这个部位的SCC和NHL的治疗方法有很大的不同。SCC通常采用手术治疗,而NHL则采用化疗、放疗或两者结合的方式治疗。因此,在治疗前准确区分这两种肿瘤是至关重要的。
作为一种无创的影像学技术,放射组学可以从常规数字医学成像中提取高维数据,已成功应用于部分头颈部肿瘤的鉴别诊断。
近日,发表在European Radiology杂志的一项研究开发并验证了一个基于增强CT(CECT)图像的包括放射组学特征和临床因素的放射组学列线图用于腭扁桃体SCC和NHL的术前鉴别诊断,为患者治疗方案的制定提供了影像学支持。
本项研究从两个临床中心招募了135名病理诊断为SCC或NHL的患者,将患者分为训练组(n = 94;SCC = 50,NHL = 44)和外部验证组(n = 41;SCC = 22,NHL = 19)。从常规CECT图像中提取的放射组学特征构建了一个放射组学特征,并计算了一个放射组学分数(Rad-score)。并利用人口学特征和CT结果建立了一个临床模型。将独立的临床因素和Rad-score结合起来构建一个放射组学列线图。使用受试者工作特性分析和决策曲线分析评估了临床模型、放射组学特征和列线图的性能。
最终选择了11个特征来构建放射组学特征。在训练(AUC,0.919 vs. 0.801,p = 0.004)和验证(AUC,0.876 vs. 0.703,p = 0.029)中,包含性别、平均CECT值和放射组学特征的放射组学列线图比临床模型对SCC和NHL的鉴别有更好的预测价值。决策曲线分析表明,放射组学列线图比临床模型更有临床意义。

A 病例 1:64 岁男性,患有鳞状细胞癌。 右侧腭扁桃体(箭头)可见肿块。 b 对肿块进行手动分割。 c 病例 2:一名 54 岁女性,患有非霍奇金淋巴瘤。右侧腭扁桃体(箭头)可见肿块。 d 手动分割肿块。
本研究建立并验证了基于CECT的放射组学列线图,其中包括性别、增强CT平均值和放射组学特征。作为一种非侵入性和定量的方法,本研究中开发的放射组学列线图可以作为鉴别腭扁桃体SCC和NHL的可靠诊断工具。
原文出处:
Cheng Dong,Ying-Mei Zheng,Jian Li,et al.A CT-based radiomics nomogram for differentiation of squamous cell carcinoma and non-Hodgkin's lymphoma of the palatine tonsil.DOI:10.1007/s00330-021-08153-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#列线图#
83
#PE#
72
#细胞癌#
66
#鉴别诊断#
79