JACC:ACEI/ARB可预防左室辅助装置相关胃肠道出血
2019-04-21 朱柳媛 中国循环杂志
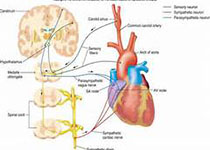
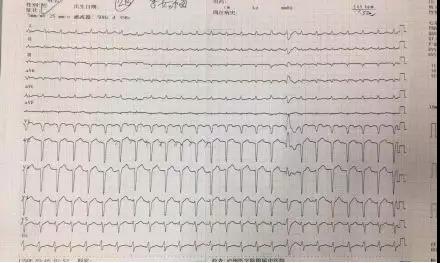
对于严重心衰患者来说,心脏移植是最好的治疗方案,但由于供体有限,很多患者需要等待。在等待心脏移植的过程中,部分患者需要机械循环支持来改善心功能、提高生活质量,其中左室辅助装置最常用。但是,安装连续流动左室辅助装置也有风险,胃肠道出血就是常见的不良事件,文献报道其发生率为15%~40%,其中高达50%的胃肠道出血与动静脉畸形有关。近期发表在JACC上的一项研究表明,血管紧张素转换酶抑制剂(ACEI)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
64
#ACE#
86
#ACC#
53
#胃肠道#
60
#胃肠道出血#
60
谢谢分享
110