J Clin Oncol:乐伐替尼治疗间变性甲状腺癌的疗效和安全性
2021-05-09 Nebula MedSci原创
乐伐替尼单药治疗可能不能有效治疗间变性甲状腺癌~
间变性甲状腺癌(ATC),一种侵袭性的恶性肿瘤,预后较差,目前尚无有效的治疗方案,特别是对于不携带BRAF突变或NTRK或RET基因融合的患者。
Lenvatinib(乐伐替尼)已获得FDA批准用于治疗放射性碘难治性的分化型甲状腺癌,也已在小规模的ATC患者研究(n=17)中被证实具有治疗活性。
本研究旨在进一步评估乐伐替尼用于ATC患者的疗效。
这是一项开放标签、国际性的、多中心的II期研究,招募了至少有一处可检测到的靶向病灶的ATC患者,予以乐伐替尼 24 mg/日
。主要终点是客观缓解率(ORR)和安全性。初次缓解4周后再次确认缓解。其他终点包括无进展生存期和总体生存期(OS)。
由于中期分析未达到15%的最低ORR阈值,该研究被提前中止。中期分析纳入了前20位患者。整体分析纳入了招募和治疗的所有34位患者。
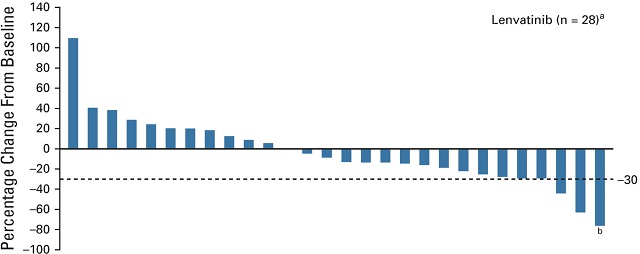
靶病灶的体积变化
在整体分析中,一位患者获得了部分缓解(ORR 2.9%,95%CI 0.1-5.3)。一半以上的可评估患者出现了肿瘤缩小;三位患者的肿瘤缩小超过了30%。
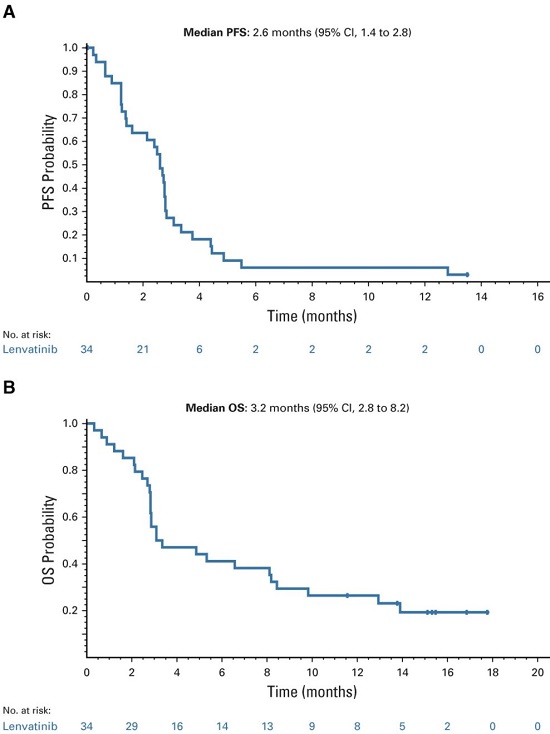
无进展生存期和总生存期
中位无进展生存期为2.6个月(95%CI 1.4-2.8);中位总生存期为3.2个月(95%CI 2.8-8.2)。
最常见的治疗相关的不良事件(AE)有高血压(56%)、食欲减退(29%)、疲劳(29%)和口腔炎(29%)。无治疗相关出血事件或5级治疗相关不良事件发生。
综上所述,乐伐替尼用于ATC患者的安全性可控,但很多不良事件导致了ATC进展。该研究结果表明,乐伐替尼单药治疗可能不能有效治疗ATC;需要进一步研究验证。
原始出处:
Lori J. Wirth, et al. Open-Label, Single-Arm, Multicenter, Phase II Trial of Lenvatinib for the Treatment of Patients With Anaplastic Thyroid Cancer. Journal of Clinical Oncology. May 07, 2021. https://ascopubs.org/doi/full/10.1200/JCO.20.03093
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#疗效和安全性#
71
#Oncol#
60
#变性#
73
谢谢梅斯提供这么好的信息,学到很多
0
谢谢梅斯分享这么多精彩信息
88
好
93