


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






5月15日JAMA刊发的一项研究报告称,在接受可植入式埋藏式心律转复除颤器(ICD)用作一级预防的无起搏适应证患者人群中发现,与应用单腔ICD相比,双腔ICD没有表现出任何优势。 这项回顾性队列研究纳入了32,000余例美国患者,其植入单腔和双腔ICD患者的1年死亡率、心衰或全因住院率均未见显著差异。丹佛健康医学中心的Pamela N. Peterson博士及其同事报告称。然而,双腔ICD却存在
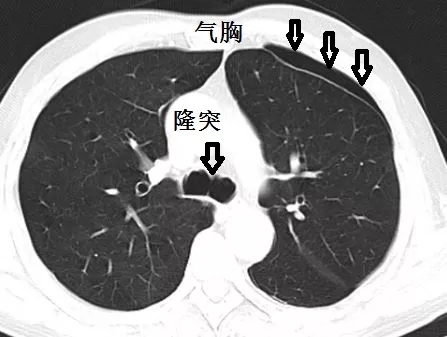
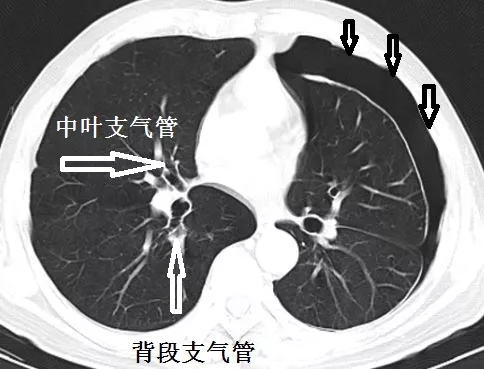
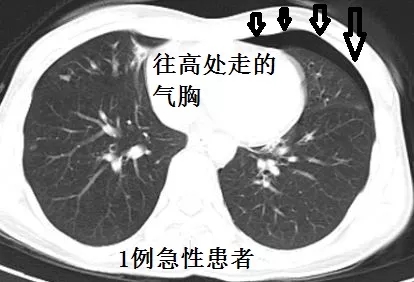
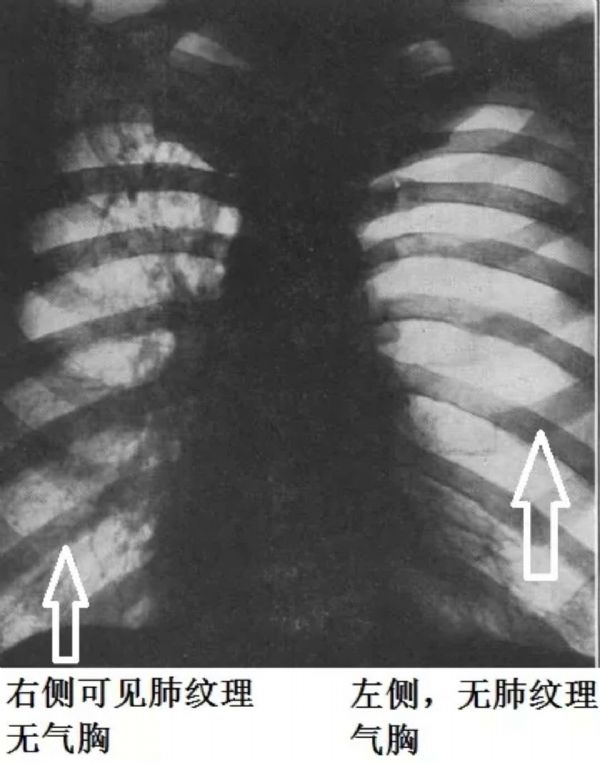
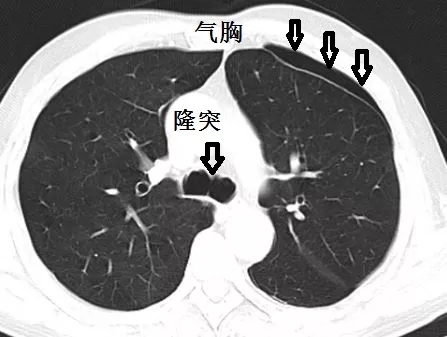
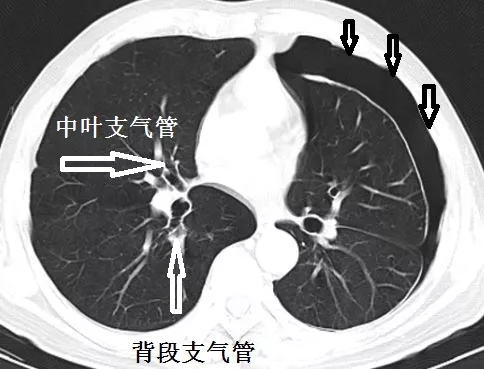
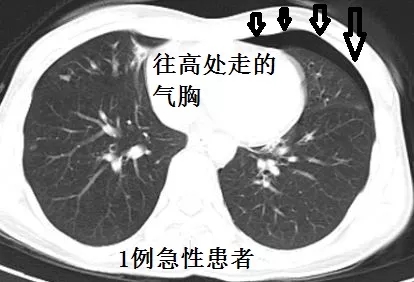
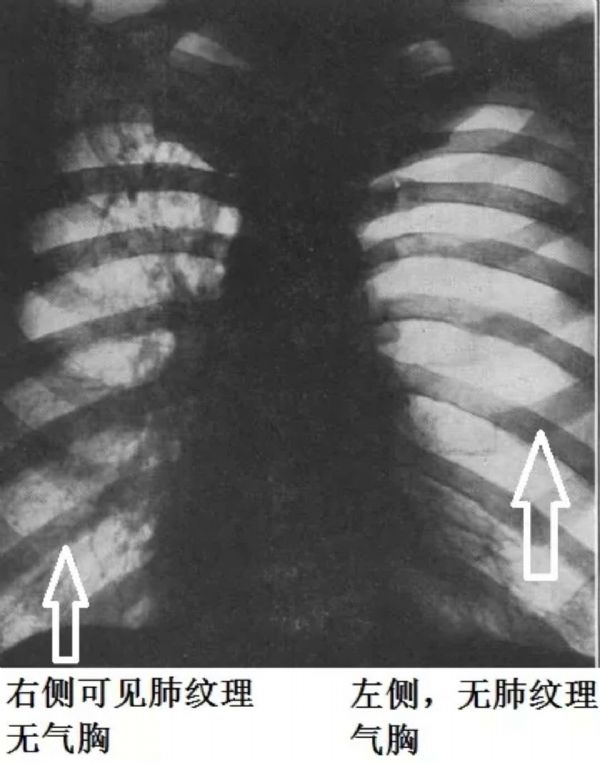
经皮肺穿刺活检是肺癌诊断的一种方法。早在数十年前就有人利用这种方法来诊断肺癌,但是由于受到当时各种条件的限制,像放射学、病理学、穿刺器械等,这种检查方法并没有在临床上得到较大的开展。本研究旨在评价经皮穿刺肺活检(PLB)后相关气胸时间依赖性发病率、危险因子和临床意义,并将结果发表在Eur Raidol上。
研究认为针吸对新生儿气胸的治疗效果优于胸腔引流,是经放射学证实的气胸患儿的首选治疗方案
一名46岁肝病终末期的女士,近来频繁地出现反复性肝性胸水和呼吸困难症状,我们对其行胸腔穿刺术治疗。在胸部检查中,右侧胸部听诊未闻及呼吸音。X线检查结果发现,右侧胸部存在液气胸(图A:箭头所指处为气胸;星号所示为胸腔积液)。我们通过猪尾导管将胸水引流出来,但气胸的问题并未能得到解决(图B所示处)。在计算机断层扫描(CT)中,结果显示右侧肺已萎缩和右侧胸膜脏层增厚,没有发现有支气管梗阻的迹象(如图C所
由此可见,该荟萃分析的结果表明PC引流可作为原发性或继发性自发性气胸患者的首选治疗方案。理想的情况下,需要进行随机对照试验来比较PC与LBCT对不同气胸患者亚组间的疗效。
美国德克萨斯大学MD安德森癌症中心的一项研究表明,经支气管肺活检(TBBX)是支气管内超声引导下的经支气管针吸活检术(EBUS-TBNA)(应用)期间引起并发症发生的唯一风险因素。快速现场细胞学评估(ROSE)显著降低TBBX的使用。该论文发表在2013年第4期《胸科杂志》[Chest. 2013; 143(4):1044-1053]。 研究者从美国胸内科医


梅斯医学MedSci APP
医路相伴,成就大医
#穿刺#
73
#气胸#
84
学习了.谢谢
113
好文献学习了
145
谢谢分享
136
了解一下.谢谢分享!
111
学习了
112