European Radiology:严重钙化的冠脉究竟要如何评估狭窄程度?CTA有了新办法!
2022-02-14 shaosai MedSci原创
冠状动脉计算机断层扫描(CCTA)是检测冠状动脉狭窄的首选无创影像学检查。然而,对于有严重钙化斑块的节段,CCTA的诊断准确性十分有限。
 冠状动脉计算机断层扫描(CCTA)是检测冠状动脉狭窄的首选无创影像学检查。然而,对于有严重钙化斑块的节段,CCTA的诊断准确性十分有限。
冠状动脉计算机断层扫描(CCTA)是检测冠状动脉狭窄的首选无创影像学检查。然而,对于有严重钙化斑块的节段,CCTA的诊断准确性十分有限。
随着最近减影CCTA(CCTASub)的发展,通过从相应的对比后CT图像数据中减去非对比CT图像数据,可以将冠状动脉钙化从图像中去除。由于该技术需要额外的后处理和辐射暴露,因此选择最适合接受CCTASub检查的病例十分重要。
然而,目前还不清楚哪些病例能从CCTAsub中获益最大。严重钙化的斑块和非严重(轻度或中度)钙化的斑块会降低CCTA的诊断准确性。
近日,发表在European Radiology杂志的一项研究使用320排CT,以有无减影信息的传统CCTA(CCTACon+Sub vs CCTACon)作为参考标准,比较了该技术在非严重和严重钙化节段应用的诊断信心、准确性和观察者间的一致性,为减影技术在临床上的进一步广泛应用提供了数据支持。
于2019年10月-2020年6月,本研究将64名疑似冠状动脉疾病(CAD)的患者(33名男性,66.6±8.2岁)纳入评估。钙化的横断面弧度被用来将钙化节段分为非严重( < 180°) 或严重钙化( ≥ 180°)。三位独立的放射学家评估了冠状动脉狭窄的严重程度。使用Fleiss'kappa (κ)评估观察者间的一致性。采用多读者多案例的受试者工作特征(ROC)方法,用ROC曲线下的平均面积(AUC)衡量诊断准确性,以≥50%的狭窄为分界点。在严重和非严重钙化的节段,比较了有无减影信息的CCTA的诊断信心、诊断准确性和观察者间的一致性。
在严重钙化的病例中(51名患者,146个节段),有减影信息的CCTA取得了更好的诊断准确性(每个患者AUC。0.73 vs 0.57,p = 0.03;每节段AUC。0.85 vs 0.62, p = 0.01)、诊断置信度(3.7 vs 2.6, p < 0.001),以及观察者之间的一致性(κ:0.59 vs 0.30)。诊断准确性(每个病人的AUC。0.81 vs 0.93, p = 0.30;每个病人的AUC。0.79 vs 0.82, p = 0.54)在非严重钙化的病例中没有增加(13名患者,190个节段)。
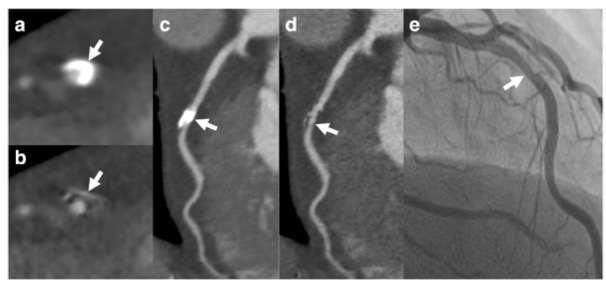
图 钙化减影法CCTA对有严重钙化(钙化截面弧度≥180°)节段的显示。左前降支中段的轴位(a)和CPR(c)图像,CCTACon上有严重的钙化负荷。CCTASub的轴位(b)和CPR(d)图像。ICA图像(e)。箭头表示钙化斑块,有无钙质减影,ICA上有相同病变。
本研究表明,CCTACon+Sub技术可增加严重钙化病变的诊断可信度、准确性和观察者间的一致性,这为该类患者的病情准确评估提供了有价值的参考依据。
原文出处:
Lixue Xu,Fang Li,Kewei Wu,et al.Subtraction improves the accuracy of coronary CT angiography for detecting obstructive disease in severely calcified segments.DOI:10.1007/s00330-021-08092-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PE#
77
学习了
95
#CTA#
79
时刻关注
73
Lihail
106