DIS COLON RECTUM:姑息性手术对 IV 期不可经手术切除的结直肠癌患者无益
2014-08-25 echo1166 丁香园
在不可经手术切除治疗的无症状 IV 期结直肠癌患者中,对原发肿瘤进行切除会给患者带来怎样的治疗效果,目前还不甚明了。 本研究的目的在于确定在无症状不可经手术切除治疗同步转移的患者中,切除原发肿瘤切除对患者预后的影响,以及确定影响肿瘤患者长期预后的影响因素。研究结果于 2014 年 9 月发布在Diseases of the Colon & Rectum上 本研究为回顾性研究。在
在不可经手术切除治疗的无症状 IV 期结直肠癌患者中,对原发肿瘤进行切除会给患者带来怎样的治疗效果,目前还不甚明了。
本研究的目的在于确定在无症状不可经手术切除治疗同步转移的患者中,切除原发肿瘤切除对患者预后的影响,以及确定影响肿瘤患者长期预后的影响因素。研究结果于 2014 年 9 月发布在Diseases of the Colon & Rectum上
本研究为回顾性研究。在 2000 年至 2008 年期间,研究者共纳入了 416 例无症状、不可经手术切除的 IV 期结直肠癌患者,并采用倾向得分匹配来进行分析。
研究者采用二元分析比较了在匹配之前的基线特征,根据 Logistic 回归估计得到的倾向得分按照 1:1 匹配了 113 对进行分析。
在 416 例患者中,有 218 例(52.4%)接受了原发肿瘤的姑息性手术切除治疗。在倾向评分匹配之前,与单因素分析所得到的结果不同,与不接受切除术的患者相比,接受姑息性手术切除治疗的受试者的生存预后更好,但是在多变量分析中,却没有得到单变量分析的结果。
在进行匹配之后,单变量分析结果提示,在存在腹膜转移和临床 M1b 期的受试者中,5 年生存率显著降低。然而,在多变量分析中,无论是腹膜转移还是临床 M1b 期都对预后无显著预测意义。
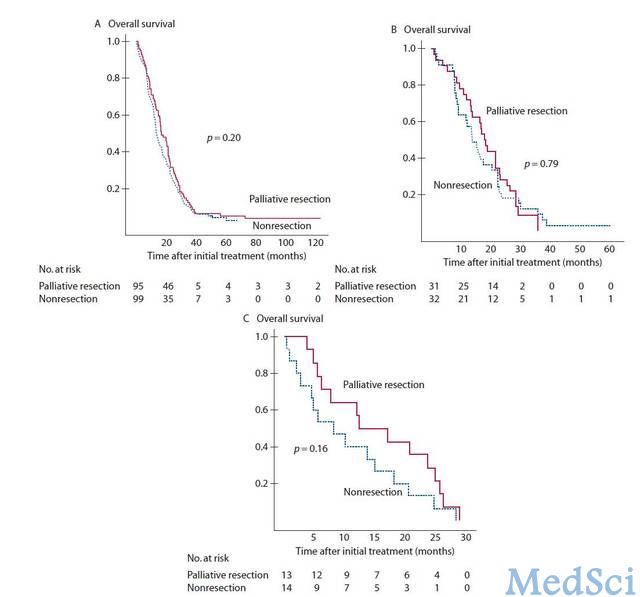
不同转移部位的生存期曲线 A 肝转移 B 肺转移 C 腹膜转移
在匹配后组中,5 年总体生存率在姑息性手术组和非手术切除组中分别为 4.9% 和 3.5%。与非手术切除组相比,姑息性切除并不能显著增加生存率。根据肿瘤转移部位所进行的亚组分析并未提示姑息性手术切除会对患者的生存带来显著获益。本研究的不足在于存在选择偏倚和潜在的混杂因素。
研究结果指出,在无症状的不可经手术切除治疗的 IV 期结直肠癌患者中,对原发肿瘤进行姑息性切除并不能改善患者的总体生存预后。
原始出处:
Yun JA1, Huh JW, Park YA, Cho YB, Yun SH, Kim HC, Lee WY, Chun HK.The Role of Palliative Resection for Asymptomatic Primary Tumor in Patients With Unresectable Stage IV Colorectal Cancer.Dis Colon Rectum. 2014 Sep;57(9):1049-58. doi: 10.1097/DCR.0000000000000193.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Dis#
0
#手术切除#
93
#结直肠#
69
#Colon#
69
#姑息#
90