Cell:复旦大学研究人员发现可雾化吸入的广谱抗新冠全人源纳米双抗药物
2022-03-11 复旦上医 网络
该双抗有望成为首个通过雾化给药方式的广谱全人源纳米抗体药物,用于新冠肺炎的特效治疗。
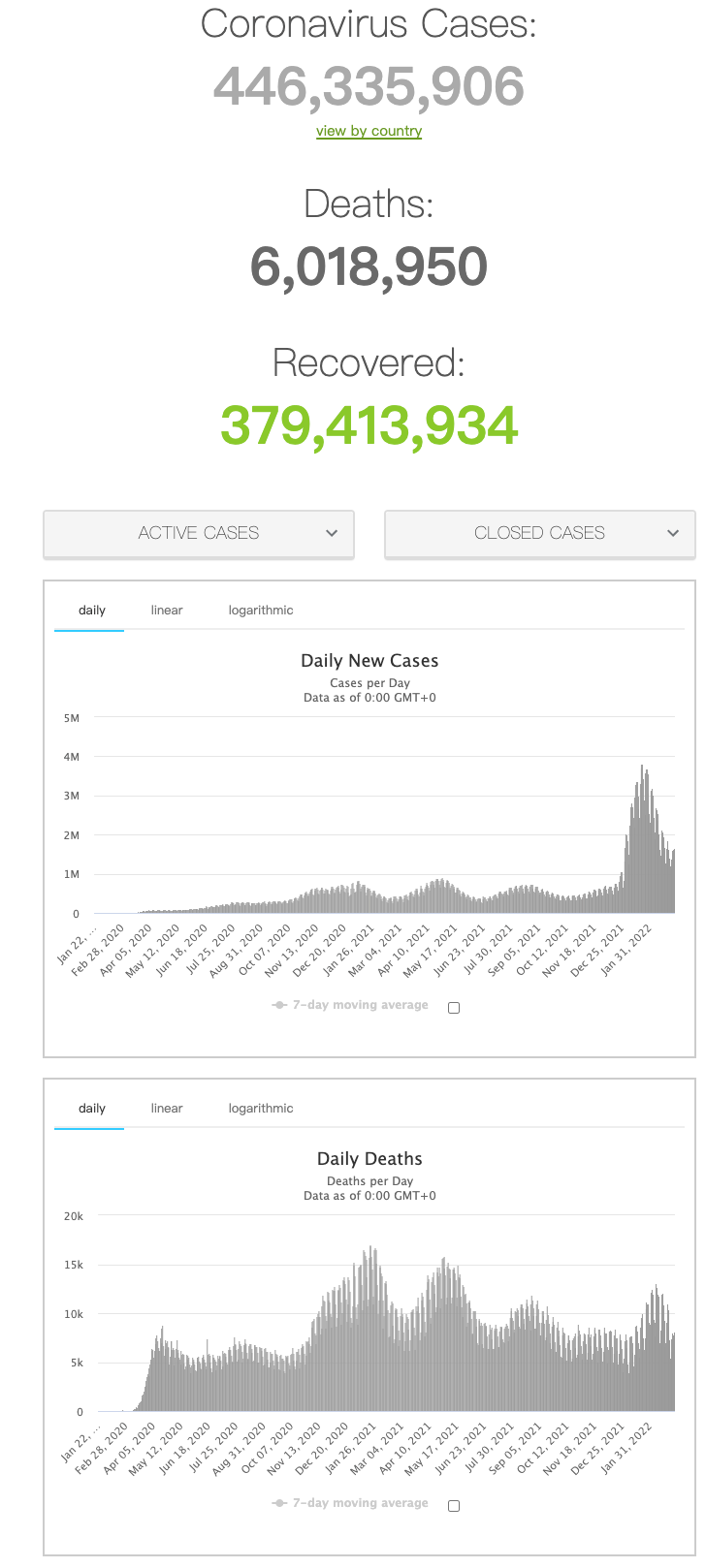
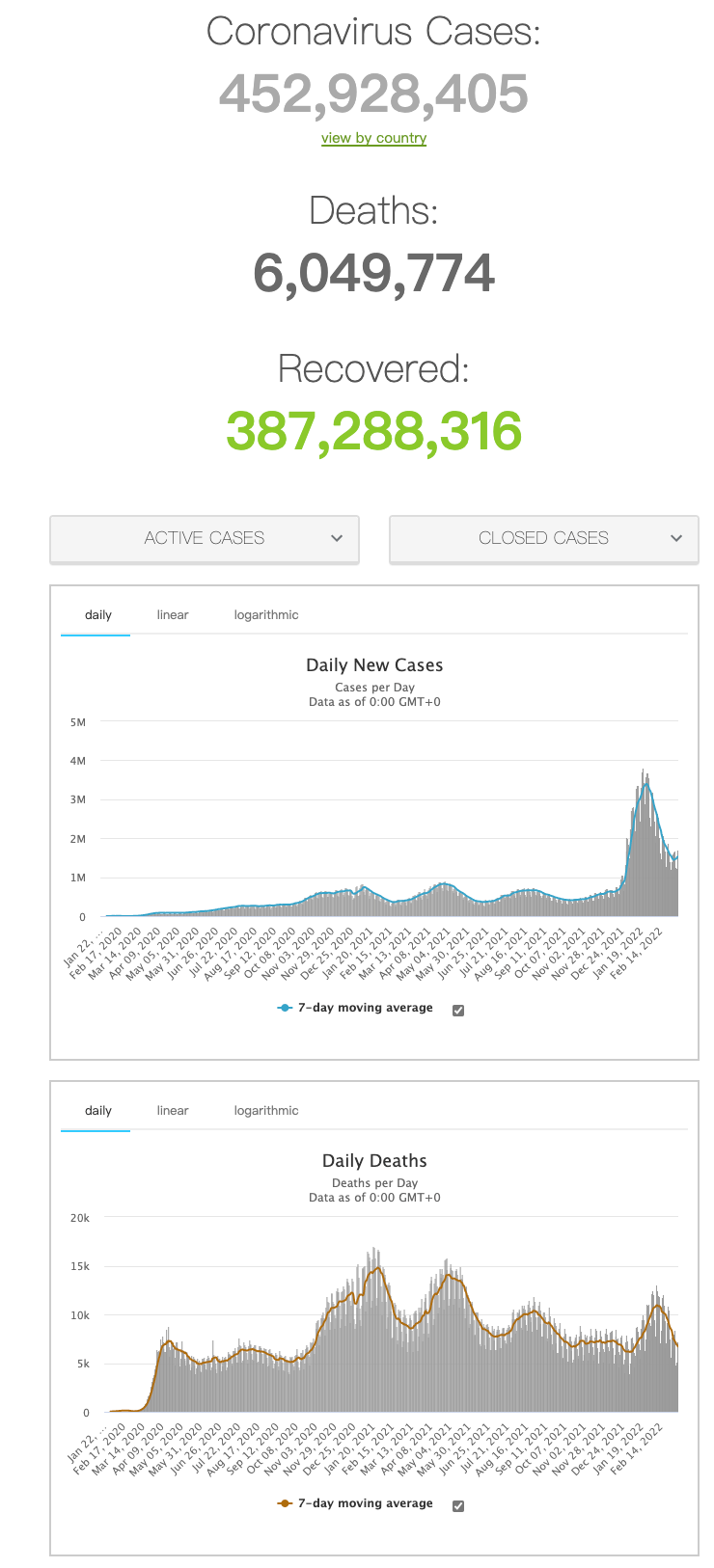
全球新冠病毒疫情形势严峻,已确定感染者超4.4亿人,死亡人数突破600万。由于新冠病毒频繁的发生突变,导致其对中和抗体和疫苗产生免疫逃逸,屡屡冲击防疫“防线”。尤其是奥米克戎变异流行株的出现,使得很多具有很好中和活性的抗体几乎完全失效,新冠疫苗的保护效果也大大被削弱。另一方面,新冠病毒的感染往往集中在呼吸道和肺部,血液中病毒很少,而单抗药物一般只能通过静脉或皮下等注射方式给药,使得抗体难以有效到达肺部。这些因素给新冠广谱疫苗和药物的研发带来了巨大的挑战。

2022年3月9日,复旦大学基础医学院应天雷与吴艳玲课题组与生物医学研究院孙蕾课题组合作,在《细胞》(Cell)杂志上发表了题为“Broad neutralization of SARS-CoV-2 variants by an inhalable bispecific single-domain antibody” 的研究论文,报道了一种抗新冠病毒的广谱双特异性全人源纳米抗体,该抗体同时靶向病毒刺突蛋白上两个不同的保守表位,能够高效中和包括奥米克戎在内的各种流行变异株。同时,该抗体具有的优良特性使其可作为雾化吸入制剂,在新冠病毒感染的轻症和重症小鼠模型中显现出很好的疗效。
自新冠疫情爆发以来,一系列新冠变异流行株迭次出现。近期在全球大范围传播的奥米克戎流行变异株(Omicron),其刺突蛋白 (Spike) 的受体结合域 (RBD) 上有多达15个突变,远超过之前出现的变异株,所以免疫逃逸能力更强。研究团队首先对Omicron的免疫逃逸特性进行了分析,发现病毒对靶向其头部受体结合区(RBM)的抗体逃逸最严重。一些已上市的针对RBM的新冠单抗已完全失效,且接种疫苗的志愿者如果血液中产生了更多的RBM抗体,则其血清对Omicron的中和活性就更弱。
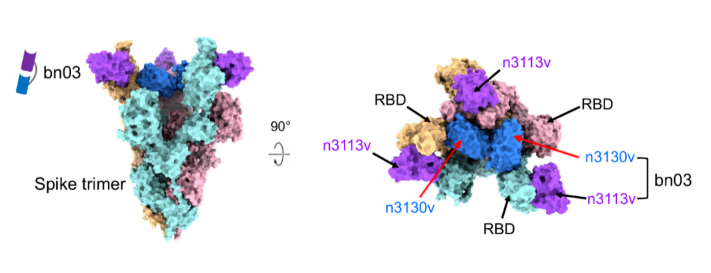
进一步,团队发现Omicron的RBD虽然发生了不少突变,但还是有两个区域未发生明显的免疫逃逸,一个是其朝向外侧的侧面区的一部分,另一个隐藏在三聚体内部。在前期研究中,应天雷团队曾建立了一种创新的全人源纳米抗体研发体系,并针对RBD不同区域筛选到了一系列高亲和力全人源纳米抗体(Cell Host Microbe, 2020)。在本论文中,团队将分别针对以上两个保守区域的两株全人源纳米抗体(n3113v和n3130v)通过适当长度的连接子串联,获得了一株分子量仅为27 kDa的小体积双特异性全人源纳米抗体(bn03),抗体理化性质优,能强效结合和中和所有的流行突变株。为了阐明抗体的作用机制,研究人员解析了全人源纳米双抗与Omicron三聚体S蛋白的结构,发现双抗两端的n3113v和n3130v可同时结合于同一个RBD上,而且一个三聚体S蛋白可同时结合3个bn03双抗。此外,n3130v的结合使“down”状态的RBD往三聚体轴线内部拉进了约13 ?,让侧面表位更多暴露,使得n3113v也能更好的结合RBD,说明了双抗的协同作用机制。更有意思的是,n3130v的表位隐藏在三聚体内部,所有的结合位点在新冠病毒高频突变株中均没有突变,是目前发现的最广谱的表位。此前团队报道的与新冠和SARS-CoV都可高亲和力结合的单抗CR3022也靶向类似表位,但n3130v和双抗bn03由于体积更小,可以更充分进入空间狭小的三聚体内部并与隐藏表位紧密结合,造成三聚体快速解体,所以具有更强的中和活性。
更重要的是,单抗等生物大分子药物往往只能注射给药,为了达到有效肺部药物浓度需要使用很高的给药剂量,增加了药物的成本和副作用的风险。与经典的单抗不同,研究团队发现全人源纳米双抗可以有效的通过雾化方式给药,形成大量中位粒径在5微米以下的雾化液滴,并且雾化后不影响双抗的活性,也不会造成双抗的降解或者聚集。在新冠病毒感染的hACE2人源化小鼠的轻症和重症模型中,雾化吸入双抗都显著降低小鼠肺部的病毒滴度并改善了肺部病理状态。
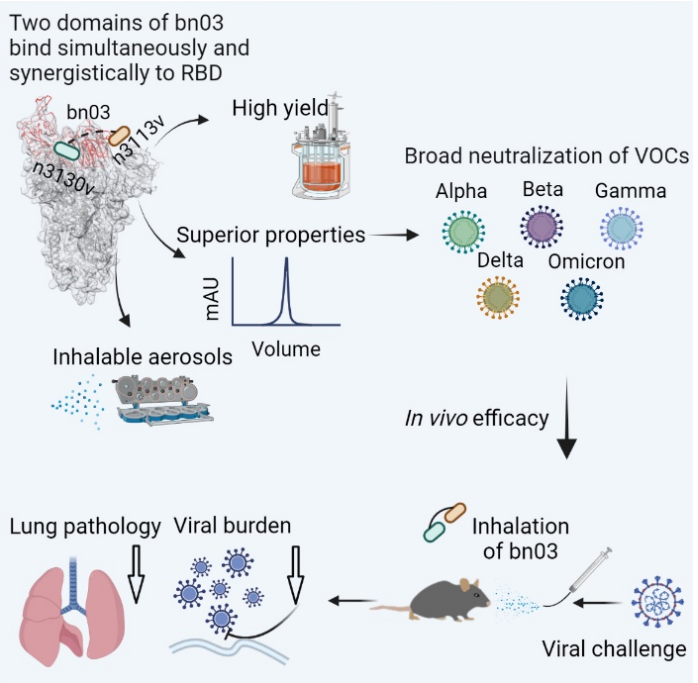
综上所述,该双抗有望成为首个通过雾化给药方式的广谱全人源纳米抗体药物,用于新冠肺炎的特效治疗。论文还发现了一类隐藏在病毒刺突蛋白三聚体内部的高度保守表位,对广谱疫苗和药物的研发具有启示作用。目前该双抗已进入中试生产阶段,正在加快向临床试验推进。
复旦大学基础医学院、上海市重大传染病和生物安全研究院应天雷研究员、复旦大学生物医学研究院孙蕾研究员、复旦大学基础医学院吴艳玲副研究员为该研究的共同通讯作者,复旦大学基础医学院博士生李澄,生物医学研究院博士生詹屋强,复旦大学附属中山医院青年研究员杨振霖,上海博奥明赛生物科技有限公司CEO涂超及复旦大学三级生物安全防护实验室胡高维为该研究的共同第一作者。该研究得到复旦大学基础医学院医学分子病毒重点实验室姜世勃教授,陆路研究员,朱园飞博士,上海博奥明赛张毅博士及复星医药崔志平先生等人的大力支持和协助。
论文链接:
https://www.cell.com/cell/fulltext/S0092-8674(22)00269-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
93
#研究人员#
132
#Cell#
74
#雾化#
91
#双抗#
141
#复旦#
92