偏头痛是一种普遍的原发性头痛疾病,直接影响着全球超过10亿人。尽管偏头痛发病率高,但目前仍没有较好的诊疗方法。为支持临床决策,Anna K. Eigenbrodt及其团队召集了一个欧洲专家小组制定了诊疗偏头痛方法,形成专家共识发布在Nature Reviews Neurology 6月刊上。每一步都由专家共识确认,并得到文献分析的支持,该共识声明已得到欧洲头痛联合会(EHF)和欧洲神经病学会(EAN)的认可。
共识内容包括偏头痛的典型临床特征、诊断标准、鉴别诊断,概述了不同人群的最佳治疗方法,包括成人、儿童、青少年、孕妇、哺乳期女性和老人。此外,声明还提供了治疗失败后如何进行评估的建议。

第一步:何时怀疑为偏头痛?
偏头痛主要分为三种主要类型:有先兆偏头痛、无先兆偏头痛和慢性头痛。
对于反复出现中度至重度头痛并伴有畏光、畏声、恶心和/或呕吐等症状的患者怀疑为无先兆偏头痛,尤其是头痛出现在单侧和/或具有搏动性时。
对于已出现上述症状,同时反复出现短暂的视觉和/或单侧感觉障碍的患者,怀疑为有先兆的偏头痛。
对于一个月内出现头痛超过15天的患者,怀疑为慢性偏头痛。尤其是对于有偏头痛家族史的,如确有慢性偏头痛,一般于青春期或青春期前后出现症状。
第二步:偏头痛的诊断
病史是偏头痛诊断的主要依据,一个完整的病史记录提供的信息应足以让医生根据ICHD-3标准作出诊断。记录病史时可运用有效的诊断辅助工具和筛查工具,如头痛日记,偏头痛鉴别问卷(ID-Migraine)和偏头痛筛查问卷。头痛日记是辅助诊疗的有效手段,用以记录有关头痛的模式、频率、症状和用药情况。请勿混淆头痛日历与头痛日记,头痛日历仅记录发病的频率、程度及头痛相关事件,用作疗效的评估(详见第七步)。
诊断时应注意与其他原发性、继发性头痛的鉴别区分,特别是一些继发性头痛严重时可能危及生命(如脑膜炎)。
神经影像学手段因为电离辐射的危害,应仅在怀疑为继发性头痛时使用。而MRI优于CT,因为MRI能提供更高的分辨率且能避免暴露于电离辐射。
第三步:教育和以患者为中心
以患者为中心和教育在偏头痛治疗中起到重要作用。医生应向每位患者解释何为偏头痛以及应对原则,包括解释偏头痛难以被治愈,降低患者不切实际的期望,指导患者如何正确地使用药物,应对不良反应。
尽管偏头痛的诱发和触发因素的重要性有限,但如果能正确识别和避免它们,无需过多干预即可实现一定的头痛控制。注意勿将加重症状的因素与诱发因素混淆,如体力活动为前者,睡眠质量差、身体素质差或压力大为后者。
第四步:急性治疗
建议为所有的偏头痛患者提供急性药物。药物的有效性与正确的时机和剂量相关,最好在头痛发作的早期使用。急性治疗可分为一线、二线、三线和辅助治疗,应采用阶梯式治疗方法。
使用非甾体抗炎药(乙酰水杨酸、布洛芬或双氯芬酸钾)作为一线药物。
使用曲坦类药物作为二线药物。如出现症状复发,可以重复使用曲坦类药物,或同时使用非甾体药物。但应告诫患者,频繁、重复地使用急性药物有发生MOH(因过度使用药物而导致的头痛)的风险。
考虑将CGRP受体拮抗剂(Gepants)和地坦作为三线药物。
使用促动力止吐药(多潘立酮或甲氧氯普胺)作为恶心和/或呕吐的辅助口服药物。
避免口服麦角生物碱、阿片类药物和巴比妥类药物。麦角生物碱效果不佳且有潜在毒性,阿片类药物和巴比妥类药物药效不定,且有相当大的副作用和依赖性。
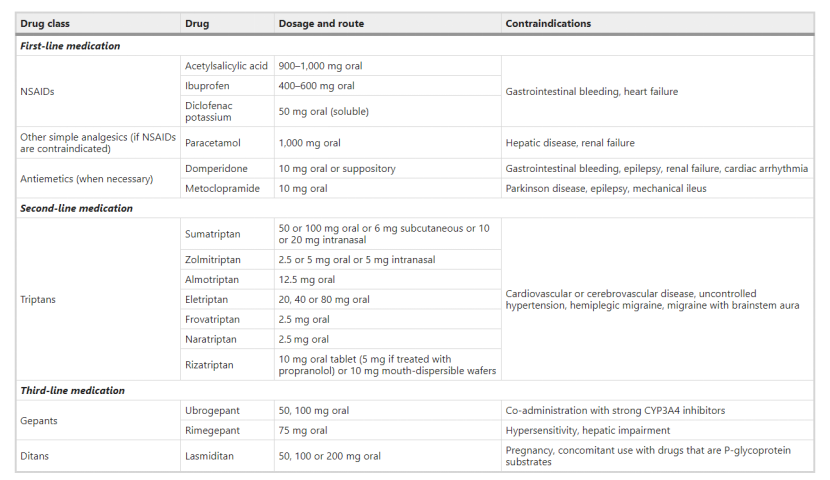
偏头痛用药一览
第五步:预防性治疗
对于尽管进行了优化了的急性治疗,但生活仍受偏头痛影响的患者应考虑额外的预防性治疗。一般对每月受到偏头痛影响大于2天的患者考虑预防性治疗,但这标准并不是绝对的,医生还应考虑偏头痛发作的严重程度、持续时间、与偏头痛相关的其他功能障碍和是否已用药过度。
预防性治疗同样可分为一线、二线和三线,实际的药物选择应根据当地的指南、是否可用和报销政策决定。
使用β受体阻滞剂(阿替洛尔、比索洛尔、美托洛尔或普萘洛尔)、托吡酯或坎地沙坦作为一线药物。
使用氟桂利嗪、阿米替林或(男性)丙戊酸钠作为二线药物。
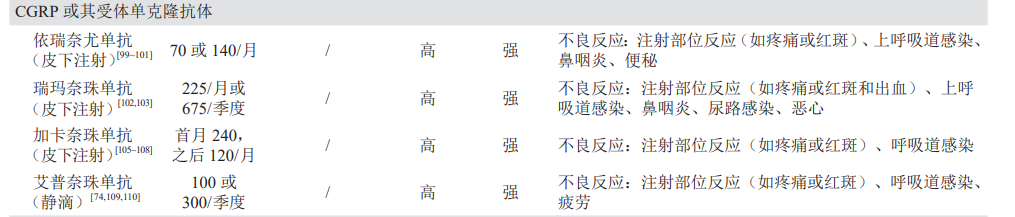
考虑将 CGRP 单克隆抗体作为三线药物。
考虑将神经调节装置、生物行为疗法和针灸作为急性和预防性药物治疗的辅助手段,或用作存在药物禁忌时的独立预防性治疗
预防性治疗起效时间较长,应劝阻患者在治疗早期因效果不明显而放弃治疗。对于口服预防性用药,在2-3个月仍无效后再考虑更换疗法,CRGP或其受体的单克隆药物评估时间为3-6个月后,肉毒杆菌毒A素药物为6-9个月后。
第六步:特殊人群偏头痛治疗
继发性头痛的发病率随着年龄增加而增加,对于年龄大于50岁的偏头痛患者,应考虑存在潜在病因,还应考虑已知和未知的合并症和药物的副作用,因为老年人往往对药物的副作用更敏感。例如不建议对老年人使用曲坦药物,因为此类患者患有心血管疾病的可能性较高。如果使用,建议定期检测患者血压、评估发生心血管疾病的风险。
偏头痛在青少年和儿童中很常见。诊断与成人一样,主要基于病史,但临床特征略有不同:发作时间同常较短,头痛更常见于双侧,胃肠道紊乱较明显。与孩子相比,父母的描述可能更可靠,也能更好地说明可能存在问题的生活方式。治疗方面,对于发作时间较短的儿童,卧床休息即可。需要时,建议使用布洛芬作为一线药物,剂量随体重调整。
对于孕期女性,需要特别考虑对胎儿的伤害。尽管疗效相对较差,扑热息痛仍应作为一线药物,曲坦类药物仅可在专家的严格监督下使用。对于妊娠期偏头痛相关的恶心,可以使用甲氧普氯胺。由于可能对胎儿造成伤害,怀孕期最好避免使用预防性药物。如实在有必要,应使用安全性最高的普萘洛尔,如有普萘洛尔使用禁忌,则使用阿米替林,二者都应在专家监督下使用。禁用托吡酯、坎地沙坦和丙戊酸钠,皆会对胎儿造成伤害。
产后的偏头痛用药也须谨慎,扑热息痛是首选急性药物,布洛芬和舒马曲坦也是安全的。如果需要预防性治疗,首选安全性最高的普萘洛尔。
大约8%的偏头痛女性患者会出现与月经有关的偏头痛发作。如果急性药物治疗不能满足需要,考虑使用围经期预防性治疗,通常为每日使用长效非甾体抗炎药或曲坦类药物,持续5天,从预期的月经前2天开始。一些无先兆偏头痛女性患者可以从连续的复合激素避孕药中获益,但对有先兆偏头痛的女性患者则会增加中风风险,应禁用复合激素避孕药。
第七步:随访、治疗效果和治疗失败时
积极的随访是确定治疗效果的最优手段,应在在开始或更改治疗方案后(2-3个月后)评估治疗效果,并在之后定期进行(每6-12个月)。评估内容包括有效性、不良反应和依从性。有效性的关键指标为发作频率、严重程度和与偏头痛有关的功能障碍。发作频率的衡量标准为每月头痛天数,严重程度为疼痛强度而不是功能性后果。可以要求患者在头痛发作时记录下来形成疼痛日历,可以用较小的投入得到较好的随访效果。当结果未达最优标准时,重新检查诊断、治疗方案、剂量和依从性。
应慎重地得出治疗失败的结论,并在之后对可能的原因进行彻底的审查。有些失败是可以补救的,比如依从性较差或剂量不合适。有些人适合大剂量,也有些人需要减少剂量来减少副作用。如果所有治疗方案均失败,应考虑诊断是否错位并咨询专家意见。
第八步:治疗并发症
应尽早提醒患者用药过度可能引发MOH。药物过度使用引起的头痛(MOH)是一种慢性头痛疾病,特征为每月头痛15天及以上。停止用药是必要且唯一的补救措施。专家共识是突然戒断比缓慢戒断更可取,阿片类等有成瘾性的药物除外。由于康复前还会经历一段恶化过程,所以应特别注意患者教育。
注意间歇性偏头痛转变为慢性偏头痛的风险。一些评估数据表明,每年有3%的间歇性头痛会转变为慢性偏头痛,治疗也随之更困难,治疗时可寻求专家意见。排除MOH的可能后,开始预防性治疗。有效的药物包括托吡酯、肉毒杆菌毒素A和 CGRP 单克隆抗体。托吡酯成本较低可作为首选。具体用药应根据当地的指南、成本和报销政策决定。
第九步:识别和治疗合并症
确保识别出偏头痛的合并症,并根据不同药之间可能产生的不良反应和并发症情况调整治疗策略。
偏头痛常常与焦虑、抑郁、睡眠障碍和慢性疼痛(如颈部和下背部疼痛)相关联。肥胖则是间歇性偏头痛转变为慢性偏头痛的危险因素。对于肥胖患者,可首选托吡酯,因为它与体重减轻有关。对于抑郁或睡眠障碍的患者,可优先选择阿米替林。
第十步:长期随访
当进行至多6个月的预防性治疗,已可见持续效果且无不良反应,制订好全面的治疗计划后即可转至一级医院,由一级医院负责偏头痛患者的长期健康管理,任务包括保障疗效的稳定和应对病情变化。
以上所有建议都基于已发表的证据和专家意见,旨在为偏头痛诊疗提供普遍适用的建议,但在临床实践时注意结合当地情况对治疗策略进行调整。
原始出处:
Harrison, S.A., Ruane, P.J., Freilich, B.L. et al. Efruxifermin in non-alcoholic steatohepatitis: a randomized, double-blind, placebo-controlled, phase 2a trial. Nat Med 27, 1262–1271 (2021). https://doi.org/10.1038/s41591-021-01425-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















学习了
91
#专家共识#
100
学习了!
92
厉害
86
学习了
106
好文章,谢谢分享
102
谢谢分享,好文章。
84