SCO-101治疗转移性结直肠癌患者的II期临床试验已开始
2019-10-05 Allan MedSci原创
Scandion Oncology制药公司近日宣布,该公司已向丹麦药品管理局提交了申请,以期允许SCO-101治疗转移性结直肠癌患者的II期临床研究,该研究将在丹麦的医院进行。
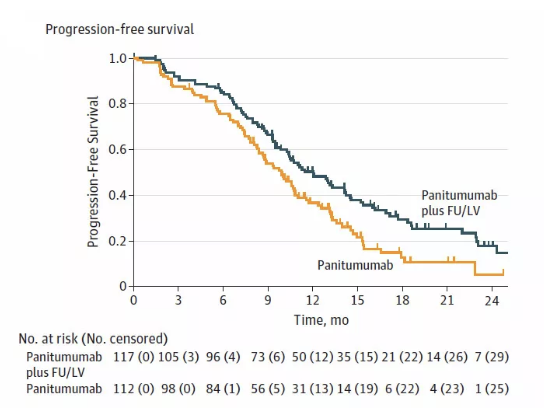
Scandion Oncology制药公司近日宣布,该公司已向丹麦药品管理局提交了申请,以期允许SCO-101治疗转移性结直肠癌患者的II期临床研究,该研究将在丹麦的医院进行。这项II期临床研究将分为两个部分进行,第一部包括12-15名患者,以证明SCO-101与化学疗法(FOLFIRI)结合使用时的安全性和耐受性。预计首批数据将于2020年第二季度发布,最终研究报告将于2021年上半年发布。
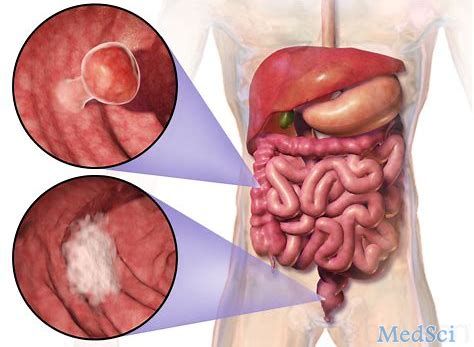
转移性结直肠癌(mCRC)患者大多不能治愈,但转移仅限于肝和/或肺、局部复发或局限性腹腔内病变的mCRC患者有手术治愈的可能。对其他mCRC患者采取姑息治疗,一般为全身化疗。
原始出处:
http://www.firstwordpharma.com/node/1671790#axzz61Rlned4y
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#II期临床试验#
91
#I期临床试验#
92
#I期临床#
61
#转移性#
93
#结直肠#
74
#II期临床#
73
期待有好的结果。
129