Diabetes:上海生科院发现糖皮质激素引起肥胖的中枢调控机制
2018-01-30 佚名 上海生命科学研究院
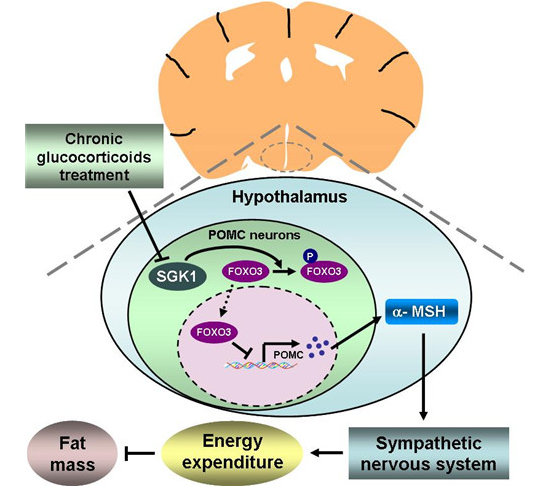
近日,中国科学院上海生命科学研究院(人口健康领域)营养代谢与食品安全重点实验室郭非凡组的研究论文,以 SGK1/FOXO3 signaling in hypothalamic POMC neurons mediates glucocorticoid-increased adiposity 为题,在线发表在 Diabetes 上,该研究发现下丘脑在慢性糖皮质激素引起肥胖中的作用与机理。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#糖皮质#
69
#上海生科院#
116
#DIA#
72
#BET#
110
#Diabetes#
155
#调控机制#
135
#皮质激素#
107
不错的文章值得推荐
0