JACC Cardiovasc Interv:陈绍良等提出冠脉复杂分叉病变新标准
2014-12-23 陈绍良等 中国循环杂志
关于如何区分冠状动脉复杂分叉病变和简单分叉病变,此前没有任何标准。 近期,南京医科大学附属第一医院陈绍良教授等在《JACC:Cardiovascular Interventions》杂志上发表的一项名为DEFINITION的研究中指出,可以通过观察患者接受经皮冠状动脉介入术(PCI)并置入药物洗脱支架1年时主要不良心脏事件(包括心源性死亡、心肌梗死和靶血管重建)发生率的高低,来区分冠脉复
关于如何区分冠状动脉复杂分叉病变和简单分叉病变,此前没有任何标准。
近期,南京医科大学附属第一医院陈绍良教授等在《JACC:Cardiovascular Interventions》杂志上发表的一项名为DEFINITION的研究中指出,可以通过观察患者接受经皮冠状动脉介入术(PCI)并置入药物洗脱支架1年时主要不良心脏事件(包括心源性死亡、心肌梗死和靶血管重建)发生率的高低,来区分冠脉复杂分叉病变和简单分叉病变。
该研究表明,冠脉分叉病变的复杂性对预后有显著的影响。分叉病变越复杂,1年时主要不良心脏事件的发生率越高。
通过分析与1年时主要不良心脏事件有关的因素,作者提出了复杂分叉病变新标准:
2个主要标准:(1)左主干远端分叉病变:分支狭窄程度≥70%,分支病变长度≥10 mm;(2)非左主干分叉病变:分支狭窄程度≥90%,分支病变长度≥10 mm。
6个次要标准:(1)中重度钙化;(2)多处病变(1、2两个因素已被证实与预后不良有关);(3)分叉角度<45度;(4)冠脉主支直径<2.5 mm;(5)病变处有血栓(通常见于急性冠脉综合征)(6)主支病变长度≥25 mm。
患者只要达到1个主要标准及任何2个次要标准,就能判定为复杂分叉病变。
该研究显示,PCI术后,复杂分叉病变患者1年内的主要不良心血管事件的发生率显著高于简单分叉病变患者,发生率分别为16.8%和8.9%。
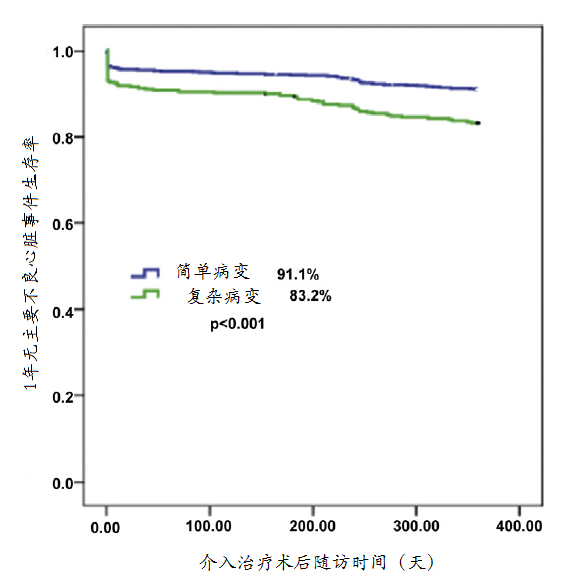
图 复杂病变患者和简单病变患者1年无主要不良心脏事件生存率比较
在复杂分叉病变的治疗上,双支架技术(主支和分支同时置入支架)和必要时支架技术(主支置入支架,分支视情况决定是否置入支架)在1年内主要不良心脏事件的发生率上没有优劣之分,分别为5% 和5.3%。
在复杂分叉病变患者中,接受双支架技术治疗者住院期间支架内血栓发生率为1%,1年内血运重建率为5.6%,而在接受必要时支架技术治疗者中上述两类事件发生率均明显降低,分别为0.2% 和3.2%。不过,与必要时支架技术相比,双支架技术治疗1年时心源性死亡(2.8% vs 5.3%)和住院期间主要不良心脏事件发生率(5.0% vs8.4%)均较低。
研究者强调,“对于简单分叉病变而言,采用越简单的技术治疗,效果越好。”在这项研究中,简单分叉病变占70%左右。
冠脉分叉病变是指冠脉主支、分支部位分别或同时存在的严重狭窄的病变,约占所有冠状动脉介入治疗的16%,术后分支再狭窄率较高,主要不良心脏事件和靶病变血运重建率也高。
这项研究纳入1500 例冠脉病变患者,共有3660 处分叉病变,所有患者接受PCI 并置入药物洗脱支架。主要终点事件为1年内主要不良心脏事件发生率,次要终点为支架内血栓形成发生率。
原始出处:
Chen SL1, Sheiban I2, Xu B3, Jepson N4, Paiboon C5, Zhang JJ6, Ye F6, Sansoto T7, Kwan TW8, Lee M9, Han YL10, Lv SZ11, Wen SY12, Zhang Q13, Wang HC14, Jiang TM15, Wang Y16, Chen LL17, Tian NL18, Cao F14, Qiu CG19, Zhang YJ6, Leon MB20.Impact of the Complexity of Bifurcation Lesions Treated With Drug-Eluting Stents: The DEFINITION Study (Definitions and impact of complEx biFurcation lesIons on clinical outcomes after percutaNeous coronary IntervenTIOn using drug-eluting steNts).JACC Cardiovasc Interv. 2014 Nov;7(11):1266-76. doi: 10.1016/j.jcin.2014.04.026. Epub 2014 Oct 15.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JACC#
55
#新标准#
88
#ASC#
91
#ACC#
77
#分叉病变#
64