J Clin Oncol:姑息性 vs 非姑息性激素使用对NSCLC免疫治疗疗效的影响
2019-07-11 Lisa 肿瘤资讯
既往的一项研究显示,在免疫治疗开始前接受≥10mg的强的松治疗与NSCLC接受PD-1单抗治疗更差的预后相关,这就引发我们思考皮质醇激素是否降低免疫治疗疗效。近日在Journal of Clinical Oncology杂志发布的另一项研究进一步评估了姑息性 vs 非姑息性激素使用对NSCLC(非小细胞肺癌)接受免疫治疗疗效的影响。
既往的一项研究显示,在免疫治疗开始前接受≥10mg的强的松治疗与NSCLC接受PD-1单抗治疗更差的预后相关,这就引发我们思考皮质醇激素是否降低免疫治疗疗效。近日在Journal of Clinical Oncology杂志发布的另一项研究进一步评估了姑息性 vs 非姑息性激素使用对NSCLC(非小细胞肺癌)接受免疫治疗疗效的影响。
研究背景
影响免疫检查点疗效的因素已经成为关注的焦点,鉴于激素类药物的免疫抑制效应以及对T细胞功能的影响,基线使用激素类药物是否影响免疫治疗的疗效值得探索。近期发布的一项研究显示,在免疫治疗开始前接受≥10mg的强的松治疗与NSCLC接受PD-1单抗治疗更差的预后相关,这就引发我们思考皮质醇激素是否降低免疫治疗疗效。然而,激素类药物主要用于缓解癌症相关症状,而这些症状本身也与更差的预后相关,如恶液质、疲劳和脑转移引发的水肿,因此,这类患者较差的预后并不一定是因为激素影响免疫治疗疗效所致。
为了评估基线激素类药物使用对NSCLC接受免疫治疗疗效的影响,研究者将患者分为3组:1)在开始免疫治疗时因为癌症相关姑息治疗适应证使用≥10mg强的松;2)在开始免疫治疗时因为非癌症相关治疗适应证使用≥10mg强的松(如自身免疫性疾病或慢阻肺或预防超敏反应或管理非癌症相关性疼痛);3)在开始免疫治疗时接受0~<10mg强的松治疗。
研究方法
研究前瞻性的收集了2011年7月至2018年9月在Dana Farber癌症中心接受PD-1/PD-L1单抗单药或联合CTLA-4抑制剂治疗的晚期NSCLC的临床病理数据。排除接受免疫治疗联合化疗的患者。纳入在首次使用PD-1/PD-L1单抗24小时内接受≥10mg强的松治疗的患者,根据其使用强的松治疗的原因分为癌症相关姑息治疗或癌症非相关的非姑息治疗。记录患者接受免疫治疗的客观缓解率(ORR)、无进展生存(PFS)和总生存时间(OS)。
研究结果
650例接受免疫治疗的晚期NSCLC患者,93例(14.3%)患者在开始首次免疫治疗24h内接受了任意口服或静脉激素治疗(等效剂量≥10mg强的松)。66例(10.25)因为癌症相关姑息治疗接受激素类药物的原因包括:有症状的脑转移(57.6%)、癌症相关气促(18.2%)、骨转移疼痛(16.7%)、癌症相关发热(7.6%)。27例(4.2%)因为非癌症相关症状接受激素类药物治疗的原因包括:既往化疗或放疗导致的肺炎(25.9%)、慢性阻塞性肺疾病管理(22.2%)、自身免疫性疾病(18.5%)、预防性碘增强显影(14.8%)和其他原因。557例接受0~<10mg激素类药物治疗的患者,仅2例接受了5mg激素类药物治疗,其余患者均未使用激素。
3组患者组年龄、性别、组织学类型、免疫检查点抑制剂治疗方案、驱动基因突变类型、PD-L1 TPS评分上均衡。与预期一致,因为癌症相关姑息治疗接受≥10mg强的松治疗的患者,PS评分更差,且免疫治疗前脑转移患者比例更高。因为非癌症相关适应症接受≥10mg强的松治疗的患者,接受二线或以上免疫治疗的患者比例更高,这可能是因为患者基线合并有自身免疫性疾病,不愿意将免疫治疗作为首选方案。TMB(肿瘤突变负荷)对比显示,接受0~10mg强的松治疗的患者,中位TMB低于接受≥10mg强的松治疗的患者。
因为癌症非相关或相关治疗适应证接受激素治疗的患者,强的松使用的中位剂量无显着差异,每日中位使用剂量分别为20mg和25mg,但激素使用时长对比,前者显着长于后者,分别为70天和35天(P=0.005)。
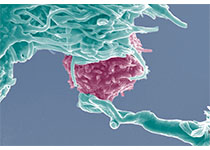
根据皮质醇适应证分析临床结局:在免疫治疗开始时,接受≥10mg强的松治疗的患者,无论其使用适应证,对比接受0~<10mg强的松治疗的患者,ORR显着更低,分别为10.8%(10/93)和19.7%(110/557),P=0.04;PFS显着更短,中位PFS分别为2.0个月和3.4个月(HR=1.36,95%CI,1.08~1.73,P=0.01);OS也显着更短,中位OS分别为4.9个月和11.2个月(HR=1.68,95%CI,1.3~2.17,P<0.01)。1562069631911680.png
研究者后续评估了强的松使用适应证对免疫治疗疗效的影响。因癌症相关姑息治疗接受≥10mg强的松的患者,相比于非癌症相关适应症接受≥10mg强的松的患者或接受0~<10mg强的松治疗患者,有显着更低的ORR,分别为6.1%、22.2%和19.7%(3组比较P<0.001);更短的PFS,中位PFS分别为1.4、4.6和3.4个月(P<0.001);更短的OS,中位OS分别为2.2、10.7和11.2个月(P<0.001)。
进一步进行两两对比发现,因癌症相关姑息治疗接受≥10mg强的松的患者相比于接受0~<10mg强的松治疗患者,PFS显着更短(HR=1.87;P<0.001);而因为非癌症相关适应症接受≥10mg强的松的患者对比接受0~<10mg 强的松治疗患者,PFS无显着差异(HR=0.77,P=0.24)。
此外,OS两两对比也具有相同的趋势,因癌症相关姑息治疗接受≥10mg强的松的患者相比于接受0~<10mg强的松治疗患者,OS显着更短(HR=2.38,P=0.001,);而因为非癌症相关适应症接受≥10mg强的松的患者对比接受0~<10mg强的松治疗患者,OS无显着差异(HR=0.93,P=0.77)。在多因素分析中,调整了ECOG PS评分和PD-L1 TPS评分后,因为癌症相关适应证接受≥10mg强的松的患者,与更高的死亡风险相关(HR=1.60,95%CI,1.07~2.39,P=0.02)。
结论和讨论
本研究结果显示,尽管在开始免疫治疗前,接受≥10mg强的松治疗的患者相比于接受0~<10mg强的松的患者,有更差的预后,但这一差异可能是因为这类患者本身就属于预后较差的人群。因此在开始免疫治疗前,没有必要减少或停止激素类药物治疗。后续需要探索使用激素治疗后是否会影响免疫活性的特定方面。
原始出处:
Ricciuti B,Dahlberg SE,Adeni A.et al.Immune Checkpoint Inhibitor Outcomes for Patients With Non–Small-Cell Lung Cancer Receiving Baseline Corticosteroids for Palliative Versus Nonpalliative Indications[J].J Clin Oncol,2019:JCO1900189.https://ascopubs.org/doi/full/10.1200/JCO.19.00189?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#非姑息性#
47
#Oncol#
53
#性激素#
51
#姑息#
73
谢谢梅斯提供这么好的信息,学到很多
73
谢谢梅斯分享这么多精彩信息
73
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
59