Blood:经典型霍奇金淋巴瘤的JAK-STAT信号通路的基因普遍存在突变
2018-04-13 MedSci MedSci原创
经典型霍奇金淋巴瘤(cHL),一种常见于青年人的癌症,由于其浸润组织中肿瘤细胞稀少(一般<5%),使得cHL的解剖病理仍充满挑战。近日,Blood杂志上发表一篇文献,研究人员通过对来自34位患者的活检组织的肿瘤和正常细胞进行显微解剖,共分离了约50000个单一的淋巴细胞,以此对cHL的编码基因进行分析。研究人员发现了几种常发生突变的基因,有STAT6(32%)、GNA13(24%)、XPO1
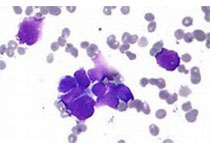
经典型霍奇金淋巴瘤(cHL),一种常见于青年人的癌症,由于其浸润组织中肿瘤细胞稀少(一般<5%),使得cHL的解剖病理仍充满挑战。近日,Blood杂志上发表一篇文献,研究人员通过对来自34位患者的活检组织的肿瘤和正常细胞进行显微解剖,共分离了约50000个单一的淋巴细胞,以此对cHL的编码基因进行分析。
研究人员发现了几种常发生突变的基因,有STAT6(32%)、GNA13(24%)、XPO1(18%)和ITPKB(16%),并记录了突变型STAT6在维持肿瘤细胞活性的功能作用。
STAT6突变与SOCS1(JAK-STAT信号通路抑制剂)破坏在遗传上和功能上存在协同作用,促进cHL生长。
总而言之,87%的病例均表现为多个基因(包括STAT3、STAT5B、JAK1、JAK2、PTPN1)遗传变异导致JAK-STAT信通路异常,证实该信号通路在cHL的发病机制中发挥关键作用,同时强调了其作为该疾病的新的治疗靶点的潜能。
原始出处:
Enrico Tiacci, et al. Pervasive mutations of JAK-STAT pathway genes in classical Hodgkin lymphoma. Blood 2018 :blood-2017-11-814913; doi: https://doi.org/10.1182/blood-2017-11-814913
本文系梅斯医学(MedSci)原创编译,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#JAK#
96
#信号通路#
94
学习了.谢谢作者分享!
131
了解一下.谢谢分享!
129