Nat Commun:癌受体蛋白结构得到解析 为药物开发铺平道路
2017-01-22 佚名 生物谷
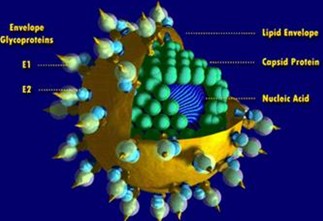
凯斯西储大学医学院的研究人员最近揭示了一种癌细胞受体蛋白的结构,未来有望用于开发对抗疾病进展的新药物。之前研究已经证明阻断该受体能够延缓一些肿瘤类型的生长和转移,但是因为很难获得这种高度不稳定的膜蛋白的结构信息,药物开发过程受到阻碍。基于该研究,药物开发者可以设计嵌入受体结合位点的分子来调节这种蛋白的功能或阻止天然配体与该受体的结合。相关研究结果发表在国际学术期刊Nature Commun
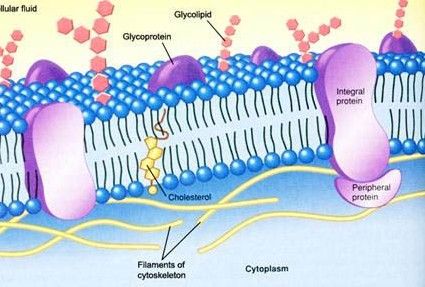
凯斯西储大学医学院的研究人员最近揭示了一种癌细胞受体蛋白的结构,未来有望用于开发对抗疾病进展的新药物。之前研究已经证明阻断该受体能够延缓一些肿瘤类型的生长和转移,但是因为很难获得这种高度不稳定的膜蛋白的结构信息,药物开发过程受到阻碍。基于该研究,药物开发者可以设计嵌入受体结合位点的分子来调节这种蛋白的功能或阻止天然配体与该受体的结合。
相关研究结果发表在国际学术期刊Nature Communications上。
在这项研究中研究人员使用了多种生化和生物信息学方法,包括最新的质谱技术,来产生ACKR3这种受体以及该受体与一种药物形成的复合体的结构模型,目前这种药物正处于2期临床试验阶段用于治疗胶质母细胞瘤。研究人员还获得了ACKR3与趋化因子相互作用的模型,这类天然小分子在体内循环控制着细胞的运动。这项工作需要获得ACKR3在多种状态下的结构形态,该分子与趋化因子的结合会导致分子形状发生巨大变化。
研究人员表示:“ACKR3是一种可以用于药物开发的抗癌和免疫系统靶标。ACKR3能够向细胞传递生长和运动信号,加速癌症发展。通过匹配该蛋白与已知激活因子和药物的相互作用,我们可以了解该分子的作用机制,包括药物结合位点以及发生相互作用后ACKR3会发生什么样的变化。”
研究人员使用了超过100种分子探针来覆盖ACKR3所有的静态和动态区域。这些探针能够帮助他们在实验室中观察到ACKR3,再拼接出ACKR3的结构。“药物的结合会导致ACKR3发生构象的变化,类似于同类的其他蛋白。这么多种受体有如此类似的机制让我们感到非常惊讶。”研究人员这样说道。
该研究提供的信息有助于对目前处于开发阶段的药物分子进行进一步筛选和提炼。
原始出处
Martin Gustavsson, Liwen Wang, Noortje van Gils, Bryan S. Stephens, Penglie Zhang, Thomas J. Schall, Sichun Yang, Ruben Abagyan, Mark R. Chance, Irina Kufareva & Tracy M. Handel.Structural basis of ligand interaction with atypical chemokine receptor 3.Nat Commun.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#COMMUN#
58
#Nat#
0
#解析#
64
#药物开发#
81
什么时候也能搞篇
134
图片好形象!
116