Eur Heart J: 急性冠脉综合征后双重抗血小板治疗中,普拉格雷+替卡格雷vs氯吡格雷
2017-05-22 MedSci MedSci原创
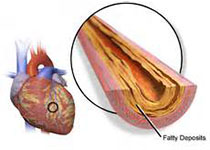
近年来急性冠脉综合征(ACS)的发病率呈上升趋势。ACS发生的关键是血小板活化聚集,我国目前治疗ACS使用最广泛的是低剂量阿司匹林联合P2Y12受体拮抗剂的方案。氯吡格雷是目前我国应用最广的P2Y12受体拮抗剂,但它是一种前体药物,存在起效 慢、药物抵抗、对P2Y12受体不逆性抑制、停药后血小板功能恢复时间长等缺点。既往的研究证明在缺血性ACS后使用新型P2Y12受体阻滞剂(普拉格雷和替卡格
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习。
110
学习。
114
学习。
95
认真学习,不断进步,把经验分享给同好。点赞了!
93
#ART#
70
#替卡格雷#
67
#双重抗血小板治疗#
64
#综合征#
0
#HEART#
76
学习了,分享了
131