Science Signaling:口腔细菌导致结直肠癌扩散?
2020-07-24 Cathy 转化医学网
导言:口腔微生物作为人体微生物群的重要组成部分,种类繁多,组成复杂。近日,弗吉尼亚理工大学的研究人员发现,一种常见的口腔细菌会导致结直肠癌细胞的扩散,并揭示了其中的机制。该研究作为封面文章发表在本期《
导言:口腔微生物作为人体微生物群的重要组成部分,种类繁多,组成复杂。近日,弗吉尼亚理工大学的研究人员发现,一种常见的口腔细菌会导致结直肠癌细胞的扩散,并揭示了其中的机制。该研究作为封面文章发表在本期《科学信号》杂志上。
先前有研究表明,严重牙龈疾病和结直肠癌之间存在联系,口腔细菌主要通过血液传播到身体的不同部位,并与大脑、肝脏和心脏的严重感染、孕妇早产有关,且在结肠肿瘤中含量很高。
近日,弗吉尼亚理工大学的研究人员发现,一种常见的口腔细菌会导致结直肠癌细胞扩散,并揭示了其中的机制。研究人员表示,90%的癌症相关死亡是由于非原发性肿瘤或转移到身体其他部位的肿瘤引起的,因此这一发现为揭示癌细胞转移的机制提供了重要信息。
该研究于7月21日发表在《科学信号》杂志。题为“Fusobacterium nucleatum host-cell binding and invasion induces IL-8 and CXCL1 secretion that drives colorectal cancer cell migration”

自2012年以来,有多项研究表明,这种细菌——具核梭杆菌(Fusobacterium nucleatum,Fn),能直接侵入结直肠肿瘤,但关于这种细菌如何导致癌症仍然存在疑问。
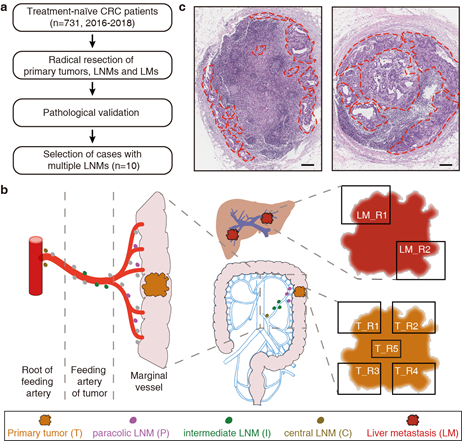
2017年的一项研究表明,将带有具核梭杆菌的人结直肠肿瘤导入小鼠体内后,含有活菌的癌细胞会脱落并重新附着在肝脏中。该研究首次证明,具核梭杆菌可能直接参与了引起癌细胞扩散以遍布全身的过程。
为了揭示具核梭杆菌促使癌细胞转移的潜在机制,弗吉尼亚理工大学的研究人员提出了一个问题:当结直肠癌细胞被具核梭杆菌感染后,人体细胞会如何反应?他们的发现为细菌在癌症中的关键作用提供了更深入的了解。
研究的起源
最初,具核梭杆菌相对温和的特性引起了Daniel Slade和他的研究小组的兴趣。乍一看,具核梭杆菌并不起眼,与口腔微生物群中牙龈下的其他细菌和谐共存。尽管它在口腔中是一种常见的细菌,但它与结肠癌的联系却十分紧密,不容忽视。
根据他们的研究,没有证据表明这种细菌会直接引发癌症。而且,这种细菌似乎也没有释放导致癌细胞迁移的分子。
然而,具核梭杆菌通过Fap2蛋白与癌细胞表面的糖类结合,以粘附细胞,甚至侵入癌细胞。这反过来又导致癌细胞释放两种蛋白质,即IL-8和CXCL1,它们是细胞因子蛋白家族的成员,在激活免疫系统抵抗感染方面起着关键作用。
值得注意的是,IL-8和CXCL1的细胞因子组合曾在多个研究中被证明可以诱导癌细胞的扩散。然而,Slade和他的团队认为,这是肿瘤相关细菌产生这种独特细胞因子组合的第一个例子。
受感染细胞释放的这些细胞因子可以与细胞本身进行交流,或者将这些信号发送给其他癌细胞、免疫细胞和肿瘤周围的各种其他细胞类型。从本质上讲,一个受感染的细胞可以影响多个相邻的细胞,所以在肿瘤内部,不一定需要存在广泛的感染,就能影响周围的大面积区域。
IL-8和CXCL1除了能使癌细胞转移外,它们也是强有力的免疫细胞引诱剂,可导致炎症,这也是癌症的标志。Slade和他的同事在这项研究中指出,具核梭杆菌吸附并感染中性粒细胞和巨噬细胞,并可能引起额外的促癌蛋白释放。李立武是生物科学系教授,同时也是弗兰林生命科学研究所的一名附属研究员,他是该研究小组在了解具核梭杆菌与免疫细胞相互作用方面的重要贡献者。
展望未来
Slade团队的长期目标是通过揭示细菌在疾病中所扮演的角色来推进癌症的治疗,这可能是这个难题中所缺失的一个关键部分。
研究发现癌细胞在遭遇细菌感染后释放促转移蛋白质,这为未来的研究打开了大门。研究结果对抑制这些细胞因子分泌的潜在方法提供了一个见解。
总之,这些结果使人们对细菌如何影响癌症有了更深入的理解。虽然这一过程被证明发生在结直肠癌细胞上,但研究小组也正在探索,是否同样的过程会影响其他类型的癌症,包括胰腺癌、乳腺癌和口腔鳞状细胞癌。

原始出处:
Michael A. Casasanta, Christopher C. Yoo1, Barath Udayasuryan, et.al. Fusobacterium nucleatum host-cell binding and invasion induces IL-8 and CXCL1 secretion that drives colorectal cancer cell migration. Science Signaling 21 Jul 2020: Vol. 13, Issue 641, eaba9157
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#signaling#
92
#Signal#
95
#Sign#
91
#SCIE#
68
#口腔细菌#
80
#结直肠#
64