Cardiovasc Diabetol:甘油三酯-葡萄糖指数与普通人心血管疾病及死亡风险的相关性
2022-07-04 MedSci原创 MedSci原创
较高的 TyG 指数可能与普通人群的冠状动脉疾病、心肌梗死和心血管疾病的发病率增加有关
心血管疾病 (CVD) 是全球普通人群过早死亡的主要原因,也是全球疾病负担的主要原因。糖尿病、高血压、肥胖和吸烟被认为是心血管疾病的重要危险因素。甘油三酯-葡萄糖 (TyG) 指数是衡量胰岛素抵抗的新替代指标。
该研究旨在评估 TyG 指数与普通人群心血管疾病和死亡率风险的相关性。
研究人员从PubMed、Cochrane Library 和 Embase 数据库检索了2022年4月16日之前收录的关于 TyG 指数与心血管疾病相关性的随机对照试验或观察性队列研究。使用随机效应模型汇总效应量。
TyG指数与普通人CAD的相关性
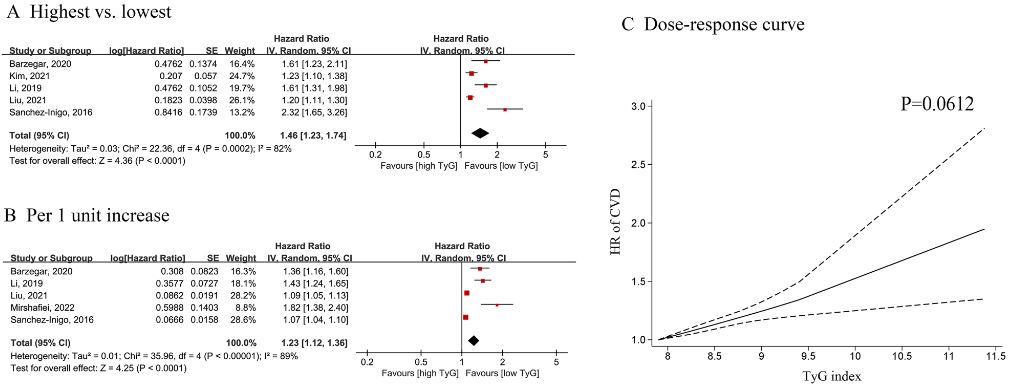
本次分析最终纳入了12个队列研究(6个前瞻性和6个回顾性队列)共6354990位受试者。与最低 TyG 指数类别相比,最高 TyG 指数与较高的冠状动脉疾病(CAD,3项研究,风险比[HR] 2.01,I2=0%)、心肌梗死(MI,2项研究,HR 1.36,I2=35%)和复合心血管疾病(CVD,5项研究,HR 1.46,I2=82%)发病率有关。
TyG指数与普通人CVD的相关性
但是,TyG 指数与死亡率(心血管死亡率,3项研究,HR 1.10, I2=76)或全因死亡率(4项研究,HR 1.08,I2=87%)无显著关联。在剂量-反应分析中,TyG 指数与 CAD(p=0.3807)或 CVD(p=0.0612)风险呈线性相关。GRADE 评估表明 CVD、MI、心血管死亡率和全因死亡率的确定性非常低,而 CAD 的确定性中等。
总之,基于以上分析,较高的 TyG 指数可能与普通人群的冠状动脉疾病、心肌梗死和心血管疾病的发病率增加有关。
原始出处:
Liu, X., Tan, Z., Huang, Y. et al. Relationship between the triglyceride-glucose index and risk of cardiovascular diseases and mortality in the general population: a systematic review and meta-analysis. Cardiovasc Diabetol 21, 124 (2022). https://doi.org/10.1186/s12933-022-01546-0.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#相关性#
83
#ASC#
76
#DIA#
60
#BET#
63
#死亡风险#
72
#血管疾病#
51