《慢性胃炎及上皮性肿瘤胃黏膜活检病理诊断共识》
2017-06-20 佚名 中华医学信息导报
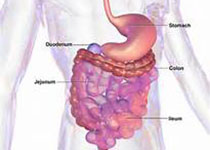
随着内镜技术的普及与发展,胃黏膜活检已成为病理诊断中最常见的项目之一。为了使病理诊断达到更好的一致性,能够准确、科学地为治疗提供参考,中华医学会病理学分会消化病理学组制定了本共识。本共识的出台,可进一步提高胃黏膜活检标本病理诊断的准确性,为临床进一步诊疗提供可靠、合理的病理依据。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#胃黏膜#
70
值得推荐一下
91
#活检#
48
#病理诊断#
49
#黏膜#
57