Science:原来,有些癌症患者天生携带响应免疫疗法的基因
2017-12-13 佚名 生物探索
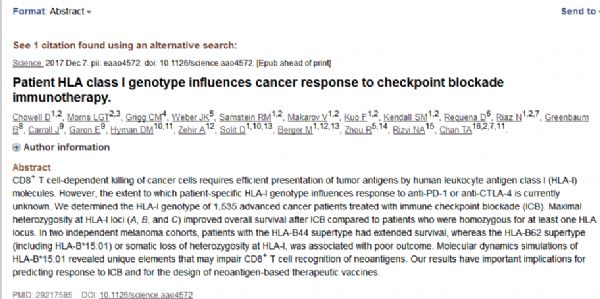
近几年,革命性的免疫疗法颠覆了癌症治疗。然而,一个不可忽视的问题是,目前,只有少部分癌症患者能够获益于这类疗法。这究竟是为什么呢?近日,来自美国Memorial Sloan Kettering癌症中心等机构的一个科学家小组发现,原来,有些癌症患者天生就携带了响应免疫疗法的基因!这篇于12月7日发表在Science杂志上的论文证实,人类白细胞抗原(human leukocyte antigen,HL
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#癌症患者#
70
#SCIE#
55
学习了.涨知识
79
谢谢分享学习了
96
学习学习
144